
greater erectile dysfunction
[98] ,short-term genitourinary
and gastrointestinal toxicity
[99] ,and long-term genitouri-
nary toxicity
[99] .Finally, there has been interest in the use
of proton EBRT, although there is little evidence of improved
oncologic or functional outcomes
[100].
In addition to the advances in EBRT delivery described,
there has been significant scientific interest in brachyther-
apy despite persistent and ongoing declines in its utilization
[101–103]. The recently reported ASCENDE-RT trial dem-
onstrated that addition of brachytherapy boost to EBRT and
ADT for men with intermediate- and high-risk disease was
associated with improved biochemical control and compa-
rable overall survival
[104]. Brachytherapy boost was
associated with greater genitourinary toxicity
[105]and
worse patient-reported overall health, sexual function, and
urinary function
[106].
4.
Conclusions
Randomized trials assessing survival following surgery or
radiotherapy in the treatment of clinically localized PCa are
significantly underpowered to address the question of
relative superiority of surgery versus radiotherapy (and
ADT) and are therefore limited in meaningfully informing
clinical practice. Observational studies of hundreds of
thousands of patients treated in clinical practice do not
support oncologic equivalence of the two modalities,
although this evidence is limited by selection bias.
Complications following PCa treatment are relatively
common. These include the commonly identified issues of
urinary incontinence and erectile dysfunction, as well as
others such as hospitalization and invasive procedures to
manage complications,
and secondary malignancies
( Table 3 ). Thus, well-powered and well-designed random-
ized controlled trials are still needed to assess the true
effectiveness of these treatments and provide definitive
answers for enhanced patient and clinician decision-making
when active treatment of localized PCa is to be undertaken.
Author contributions:
Christopher J.D. Wallis had full access to all the
data in the study and takes responsibility for the integrity of the data and
the accuracy of the data analysis.
Study concept and design:
Wallis, Glaser, Hu, Huland, Lawrentschuk,
Moon, Murphy, Nguyen, Resnick, Nam.
Acquisition of data:
Wallis.
Analysis and interpretation of data:
Wallis, Glaser, Hu, Huland, Law-
rentschuk, Moon, Murphy, Nguyen, Resnick, Nam.
Drafting of the manuscript:
Wallis.
Critical revision of the manuscript for important intellectual content:
Wallis,
Glaser, Hu, Huland, Lawrentschuk, Moon, Murphy, Nguyen, Resnick, Nam.
Statistical analysis:
None.
Obtaining funding:
None.
Administrative, technical, or material support:
Nam.
Supervision:
Nam.
Other:
None.
Financial disclosures:
Christopher J.D. Wallis certifies that all conflicts of
interest, including specific financial interests and relationships and
affiliations relevant to the subject matter or materials discussed in the
manuscript (eg, employment/affiliation, grants or funding, consultan-
cies, honoraria, stock ownership or options, expert testimony, royalties,
or patents filed, received, or pending), are the following: Jim C. Hu has
received speaker fees from Intuitive Surgical and Genomic Health.
Declan G. Murphy has received advisory and speaker fees fromAstellas,
Janssen, Ipsen, Sanofi, and Ferring. Paul L. Nguyen has received
consulting fees from Ferring, Medivation, Genome Dx, Dendreon, and
Nanobiotix, and research funding from Astellas and Janssen. The
remaining authors have nothing to disclose.
Funding/Support and role of the sponsor:
None.
Acknowledgments:
Christopher J.D. Wallis is supported by a Canadian
Institute of Health Research Banting and Best Doctoral Award. Robert K.
Nam is supported by the Ajmera Family Chair in Urologic Oncology.
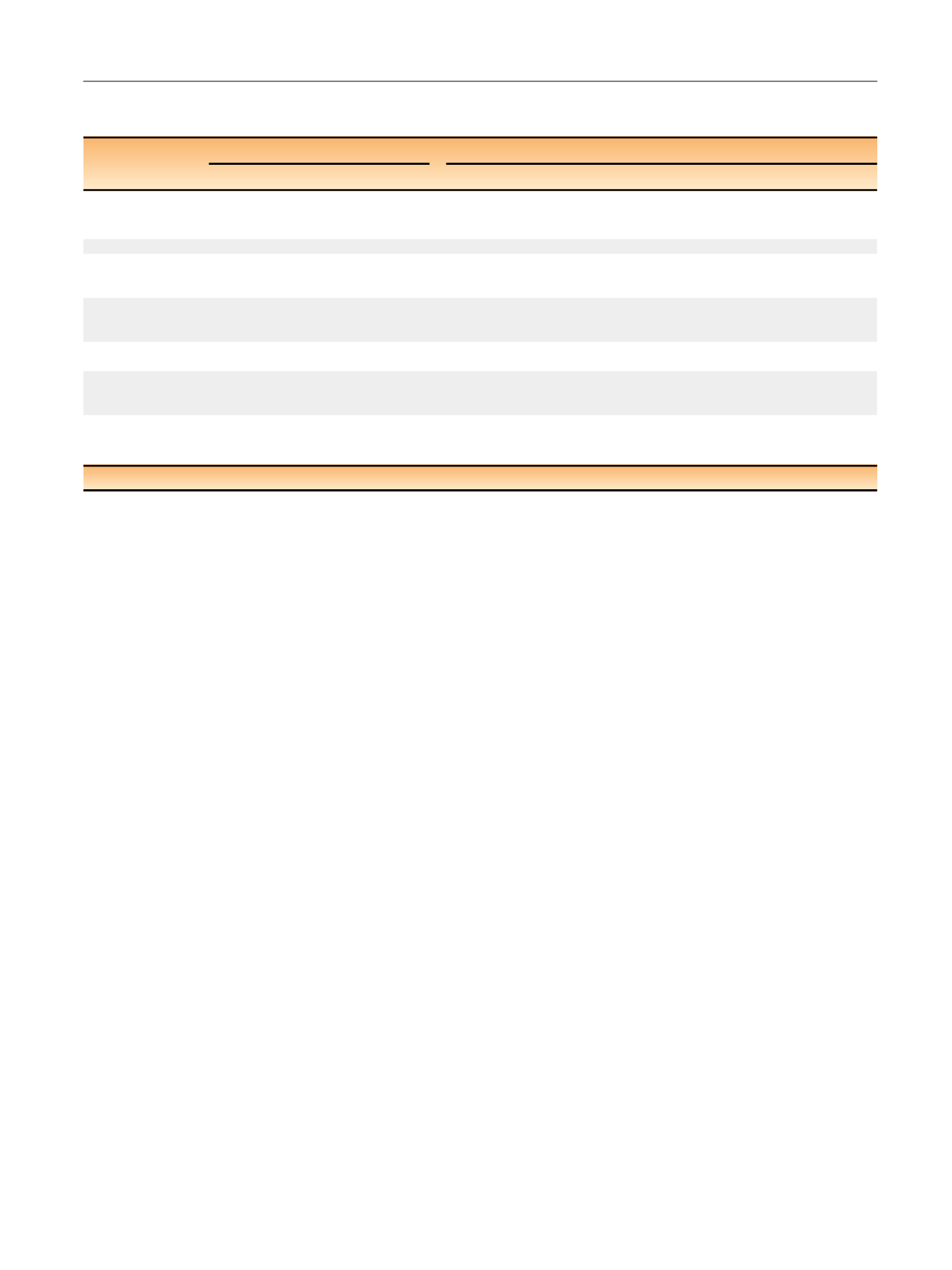
Table 3 – Comparison of key outcomes following radical prostatectomy and radiotherapy in the treatment of localized prostate cancer,
stratified by evidentiary study design
Outcome
Randomized controlled trials
Observational cohort studies
Evidence
Caveats
Evidence
Caveats
Survival
No difference
Underpowered and
over-representation
of low-risk patients
Significantly better overall and prostate cancer–
specific survival for patients treated with surgery
Residual confounding, with study
design unable to fully account for
baseline differences
Global HRQoL
No difference
–
No difference
Residual confounding
Urinary function
Conflicting evidence:
probably no
long-term differences
–
Greater incontinence early after surgery and
greater urinary bother after RT; no differences
long term
Residual confounding
Erectile function
Conflicting evidence:
probably no
long-term differences
–
Worse erectile function early after surgery; no
difference long term
Residual confounding
Bowel function
Worse after RT
–
Worse bowel function early after RT; no
difference long term
Residual confounding
Other complications No data
Higher risk of urologic and rectal-anal
procedures, major surgeries, and hospitalization
to manage treatment-related effects after RT
Residual confounding
Secondary
malignancies
No data
Higher risk of bladder, rectal, and colorectal
cancer after RT
Despite significant relative risk,
small absolute risk; residual
confounding
[1_TD$DIFF]
HRQoL = health-related quality of life; RT = radiotherapy.
E U R O P E A N U R O L O G Y 7 3 ( 2 0 1 8 ) 1 1 – 2 0
17
















