
 Table 1
Table 1
lists the symptoms present in each patient and
instrumental findings.
Seven of the patients presented with a history of multiple
urethral dilatations. One also had a previous internal
urethrotomy. Another patient had a previous intervention
due to urethral stricture using the Blandy’s technique, with
a stricture recurrence 2 yr afterwards. The last patient was
treated for a third degree cystocele. In this latter case, the
cystocele was successfully treated, although the urinary
symptoms remained.
Voiding cystourethrography gave rise to two different
results. Six of the patients presented with a narrow urethral
segment, with a dilated proximal urethra and bladder neck
during micturition
( Fig. 2 ). The whole urethra of the three
remaining patients was strictured, reaching up to 1 cm of
the bladder neck and remaining so throughout the whole
time of exploration
( Fig. 3 ). Also, three patients presented
with bladder trabeculation with cellule formation.
Eight women recovered favorably following catheter
removal. The remaining patient required catheter drainage
for 4 wk. However, after removing the catheter, bladder
function was recovered and the patient was subsequently
able to void normally with no recurrent stricture.
Concerning maximum urinary flow, median values were
6.8 ml/s before the surgical procedure and 21 ml/s in the
last follow-up (
p
<
0.01). The median peak flow difference
was 14.2 ml/s (3–35 ml/s) and the median ratio was 3:1.
No immediate or delayed complications or lasting side
effects appeared after surgery. Six of the patients remained
sexually active. The sexual inactivity of the other three
patients was not related to the intervention.
Table 1lists the
postoperative and preoperative results.
4.
Discussion
FUS is a relatively rare condition, with an approximate
prevalence of 15% of cases with bladder outlet obstruction,
although its true prevalence is still largely unknown
[14] .Etiology is identifiable in only 50% of the cases
[10] .In our
study, four of our nine patients presented with FUS due to a
physical trauma with instrumentation, with another two
describing complications while giving birth.
A proper diagnosis is difficult, as the symptoms are often
nonspecific and there is currently no consensus on the
diagnostic criteria for FUS. Subsequently, diagnosis gener-
ally relies on the use of a multitude of tests.
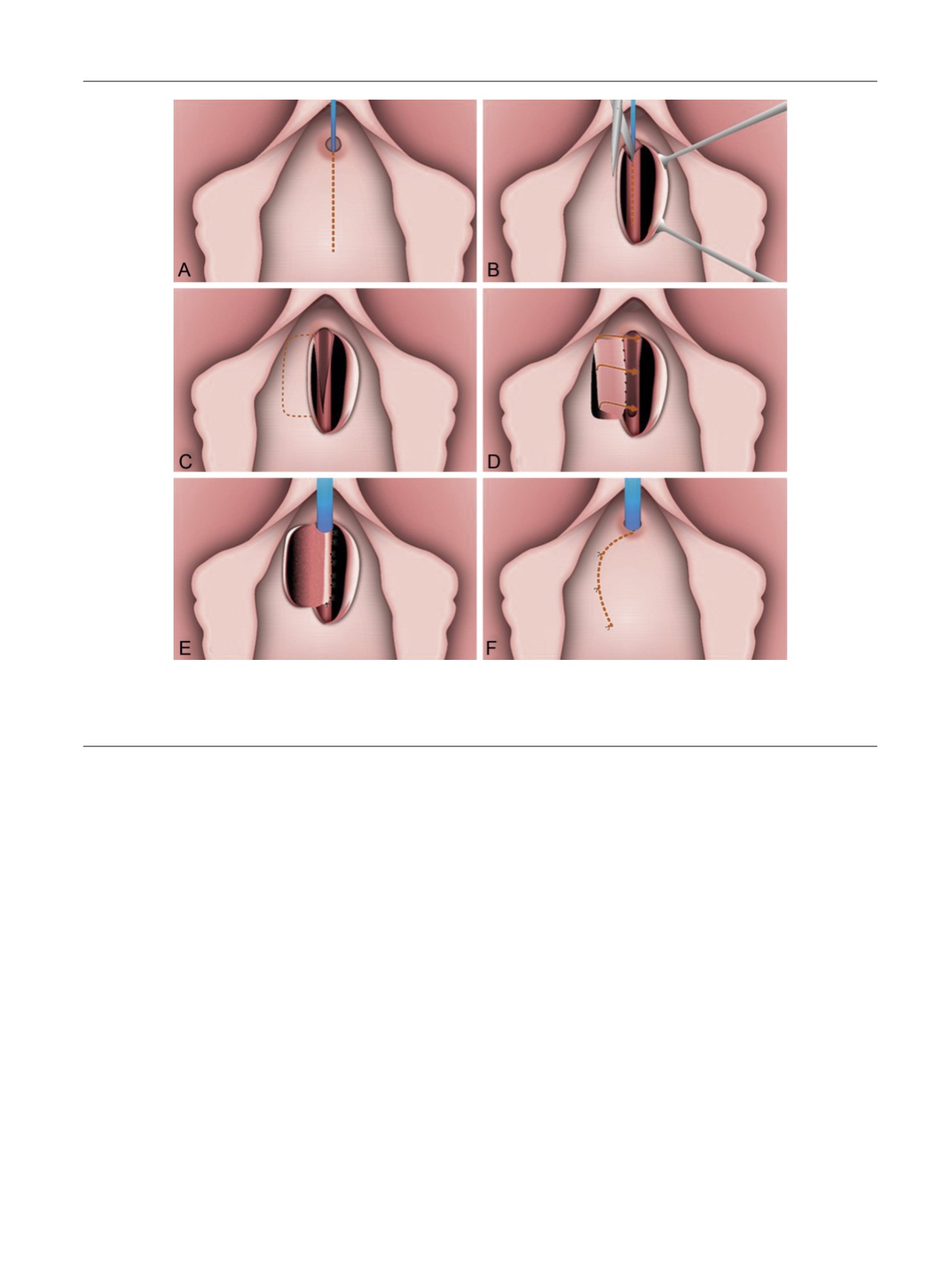
[(Fig._1)TD$FIG]
Fig. 1 – Surgical procedure. A: Midline anterior vaginal wall incisio´n. B: After mobilization of anterior vaginal wall, the urethra is incised ventrally from the
meatus to the point where the stricture is completely open. C: A rectangular-shaped piece of vaginal wall is then selected and the outer external flap border
is mobilized with a wide vascular pedicle. D: The vaginal flap is sutured to the margins of the urethrotomy defect. The inner vaginal flap edge to the closer
urethral margin. E: The outer vaginal flap edge is turned around and sutured to the contralateral edge. F: The vaginal mucosa has been approximated.
E U R O P E A N U R O L O G Y 7 3 ( 2 0 1 8 ) 1 2 3 – 1 2 8
125
















