
Abiraterone or Docetaxel for Castration-sensitive Metastatic
Prostate Cancer? That Is the Question!
Carlo Messina
a[5_TD$DIFF]
, b , * , Marco Messina c , Francesco Boccardo a , bAndrogen deprivation therapy (ADT), using bilateral orchi-
ectomy or luteinizing hormone
–
releasing hormone agonist
or antagonist, represented for many decades the standard of
care for both locally advanced prostate cancer (PCa) and
metastatic PCa (mPCa). Results from two of three large
randomised phase III trials
[1 – 3](CHAARTED, STAMPEDE,
and GETUG-AFU15 trials) showed an absolute improvement
in 4-yr survival of 9% from the combination of docetaxel and
ADT in hormone-sensitive mPCa. Abiraterone plus predni-
sone and ADT improved overall survival (OS) in castration-
resistant mPCa in either pre- or post-docetaxel setting.
However, the efficacy of this agent in hormone-sensitive
mPCa was until recently unknown. Two recently published
phase III randomised controlled trials
—
LATITUDE
[4]and
STAMPEDE
[5]trials
—
have assessed the efficacy of abir-
aterone and prednisolone plus ADT versus ADT alone in
castration-sensitive mPCa and in newly diagnosed mPCa,
and node-positive and high-risk locally advanced non-
mPCa, respectively. Hence, we performed a meta-analysis
to assess the clinical benefit of abiraterone plus ADT and
the pooled impact of abiraterone and docetaxel on the
subgroup of castration-sensitive mPCa. OS and progression-
free survival (PFS) data were extracted from five phase III
trials available. Random-effect models were used for
pooling data to account for heterogeneity in these studies.
Analysis was performed using Cochrane RevMan version
5.2 software (Cochrane Tech, London, UK). A total of
2201 patients (1097 abiraterone + ADT and 1104 ADT) were
included. Patients treated with abiraterone and ADT
achieved a significant improvement in OS (hazard ratio
[HR]: 0.62; 95% confidence interval [CI] 0.53
–
0.71;
p
<
0.001), PFS (HR: 0.38, 95% CI 0.25
–
0.57,
p
<
0.001),
and time to next symptomatic skeletal event (HR: 0.55, 95%
CI 0.46
–
0.65,
p
<
0.001;
Table 1). Despite the methodologi-
cal limitation concerning the indirect comparison of results
achieved adding ADT to abiraterone or docetaxel, abirater-
one plus ADT might provide slightly better OS (HR: 0.62 vs
0.73) and PFS (HR: 0.38 vs 0.63) than docetaxel plus ADT.
Pooling together the results of the five phase III trials, we
confirm that abiraterone or docetaxel plus ADT provides
meaningful outcome compared with ADT alone (OS, HR:
0.67, 95% CI 0.59
–
0.77; PFS, HR: 0.51, 95% CI 0.39
–
0.68) in
castration-sensitive mPCa. These data reinforce the role of
both drugs in castration-sensitive mPCa, and the different
mechanisms of action constitute the rationale to design
new trials evaluating the efficacy of their combination plus
ADT in this setting.
Although an individual patient data meta-analysis should
be performed, our results highlight that early administration
of abiraterone plus ADT improves clinical outcomes com-
pared with ADT and represents an alternative option to
chemohormonal treatment. Emerging data provide a new
opportunity, especially for elderly patients with poor
performance status or coexisting illnesses, and benefit
should be balanced with longer treatment duration and
costs. Based on the results of current trials, the question of
what should be regarded as the standard of care for
castration-sensitive mPCa is still unanswered. Head-to-head
trials are warranted to compare the efficacy of upfront
treatment with abiraterone or docetaxel plus ADT, improve
patient selection, and maximise the benefit from the two
strategies with a favourable balancewith toxicities and costs.
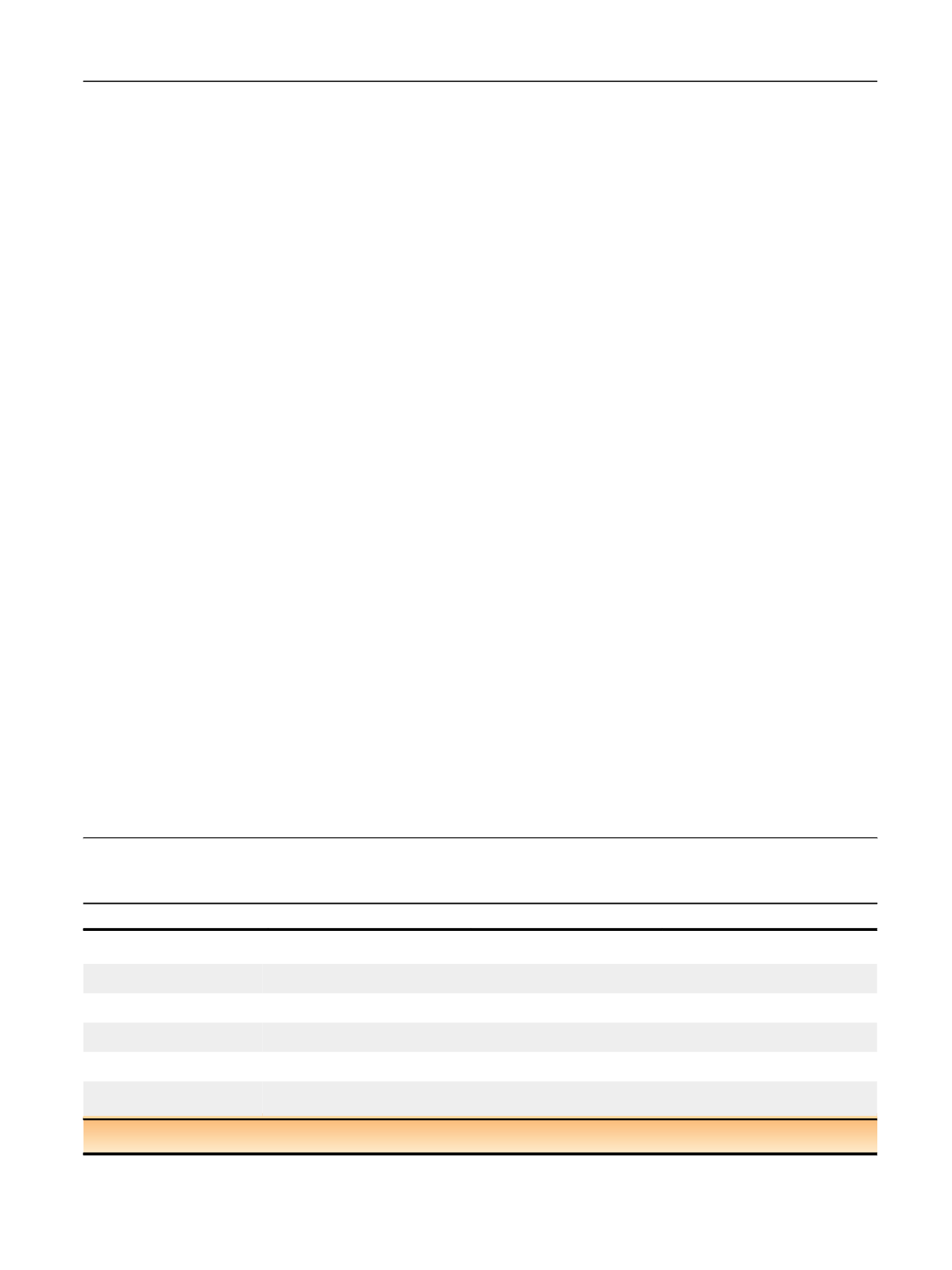
Table 1
–
Comparison between hazard ratios (HRs) for overall survival (OS) and progression-free survival (PFS) from five randomised phase
III clinical trials of abiraterone plus androgen deprivation therapy (ADT) compared with ADT, docetaxel plus ADT compared with ADT, and
abiraterone/docetaxel plus ADT compared with ADT in patients with metastatic hormone
–
sensitive prostate cancer
Treatment under investigation
Abi + ADT versus ADT
Doc + ADT versus ADT
Abi/Doc + ADT versus ADT
Trials included for the
pooled analysis
LATITUDE [4], STAMPEDE [5]
CHAARTED [1], STAMPEDE [2],
GETUG-AFU15 [3]
LATITUDE, STAMPEDE, CHAARTED [1],
STAMPEDE [2], GETUG-AFU15 [3]
Number of patients
2201
(1097 vs 1104)
2951
(1181 vs 1770)
5152
(2278 vs 2874)
Pooled HR for OS
HR = 0.62
95% CI 0.53
–
0.71,
p
<
0.001
HR = 0.73
95% CI 0.60
–
0.90,
p
= 0.02
HR = 0.67
95% CI 0.59
–
0.77,
p
<
0.01
Heterogeneity test for OS
t
2
= 0.0;
x
2
= 0.0; df = 1 (
p
= 0.95);
I
2
= 0%;
Z
= 6.55 (
p
<
0.00001)
t
2
= 0.02;
x
2
= 3.88; df = 2 (
p
= 0.14);
I
2
= 49%;
Z
= 3.05 (
p
= 0.002)
t
2
= 0.01;
x
2
= 6.28; df = 4 (
p
= 0.18);
I
2
= 36%;
Z
= 5.96 (
p
<
0.00001)
Pooled HR for PFS
HR = 0.38
95% CI 0.25
–
0.57;
p
<
0.001
HR = 0.63
95% CI 0.57
–
0.70;
p
<
0.001
HR = 0.51
95% CI 0.39
–
0.68;
p
<
0.001
Heterogeneity test for PFS
t
2
= 0.08;
x
2
= 10.38; df = 1 (
p
= 0.001);
I
2
= 90%;
Z
= 4.71 (
p
<
0.00001)
t
2
= 0.00;
x
2
= 0.84; df = 2 (
p
= 0.86);
I
2
= 0%;
Z
= 8.31 (
p
<
0.00001)
t
2
= 0.09;
x
2
= 41.93; df = 4 (
p
<
0.00001);
I
2
= 90%;
Z
= 4.68 (
p
<
0.00001)
Abi = abiraterone; CI = con
fi
dence interval; df = degree of freedom; Doc = docetaxel.
Pooled HRs were computed using random-effect models.
E U R O P E A N U R O L O GY 7 3 ( 2 0 18 ) 14 5
–
14 8
147
















