
1.
Introduction
Multiparametric magnetic resonance imaging (MPMRI) is
increasingly being recommended for the diagnosis of
clinically significant (CS) prostate cancer, if the initial
biopsy proves negative
[1,2]. An alternative approach is to
begin with MPMRI imaging to inform who needs a biopsy
and, in those who need it, how it might be best conducted
[3] .Recent studies have reported encouraging results on the
performance of MPMRI in detecting CS prostate cancer
[3 – 5] .The Prostate MR Imaging Study (PROMIS) was the largest
accuracy study on the use of MPMRI and transrectal
ultrasound-guided biopsy (TRUSB) in the diagnosis of
prostate cancer
[4] .Using template mapping biopsy (TPMB)
as the reference standard, it was found that MPMRI had
better sensitivity for CS prostate cancer compared with
TRUSB but worse specificity
[4]. It is therefore necessary to
explore how best to combine these tests and the
consequences of incorrect diagnosis on health outcomes.
This study aims to identify the combinations of tests
—
diagnostic strategies
—
that detect the most CS cancers per
pound spent in testing and achieve the maximum health
given their cost to the healthcare service.
2.
Patients and methods
The target population was men at risk of prostate cancer referred to
secondary care for further investigation
[4,6] .The perspective was the
UK National Health Service (NHS). Costs were expressed in pound
sterling from a 2015 price base. The time horizon is the population
’
s
predicted lifetime. Costs incurred and health outcomes attained in the
future were discounted to present values at 3.5% per annum
[7] .2.1.
Diagnostic strategies
The diagnostic strategies consisted of clinically feasible combinations of
MPMRI, TRUSB, and TPMB, in addition to the use of TRUSB and TPMB in
isolation
( Table 1; details in the Supplementary material, section 1.1).
These included strategies using MPMRI to decide whether a TRUSB or
TPMB is necessary and target the TRUSB, and strategies starting with
TRUSB and using MPMRI to decide whether a repeat biopsy is warranted.
A diagnosis of CS cancer requires a biopsy, hence strategies were de
fi
ned
to always end with a con
fi
rmatory biopsy. Within each test combination,
there are alternativeways each test can be used, following the de
fi
nitions
used in PROMIS (see
Tables 2 and 3). Each of the 32 test combinations
were tested for the alternative classi
fi
cations and cut-offs, returning a
total of 383 strategies.
2.2.
Model structure
The model had a diagnosis and a long-term component (Supplementary
Fig. 1). For diagnosis, a decision tree combined the information on
diagnostic accuracy of the tests to determine the accuracy of the test
combinations
( Fig. 1). The long-term outcome component calculated the
long-term health outcomes and costs of men with CS cancer, non-CS
cancer, and no cancer, by whether they were correctly diagnosed or
missed. Their diagnosis determined their clinical management, as either
immediate radical treatment if CS cancer is diagnosed or surveillance if
not. The long-term outcome component was a cohort Markov, with two
health states for menwith no cancer (alive and dead) and three states for
men with cancer: localised cancer, metastatic cancer, and death. The
decision model was developed in Microsoft Excel.
2.3.
Diagnostic performance
The model explicitly re
fl
ects the sensitivity and speci
fi
city of TRUSB and
MPMRI in detecting prostate cancer.
Tables 2 and 3show the diagnostic
performance of the tests, calculated from the individual level data
collected in the PROMIS
[4](details in the Supplementary material,
section 2). The men
’
s true disease status was classi
fi
ed in four subgroups,
according to the TPMB results and their serum prostate-speci
fi
c antigen
(PSA) level
[1]:
1. No cancer
2. Low risk: PSA 10 ng/ml and Gleason score 6, who should be
classified as having non-CS cancer
Patient summary:
We found that, under certain assumptions, the use of multiparametric
magnetic resonance imaging
fi
rst and then up to two transrectal ultrasound-guided biopsy
is better than the current clinical standard and is good value for money.
© 2017 European Association of Urology. Published by Elsevier B.V. This is an open access
article under the CC BY license
( http://creativecommons.org/licenses/by/4.0/ ).
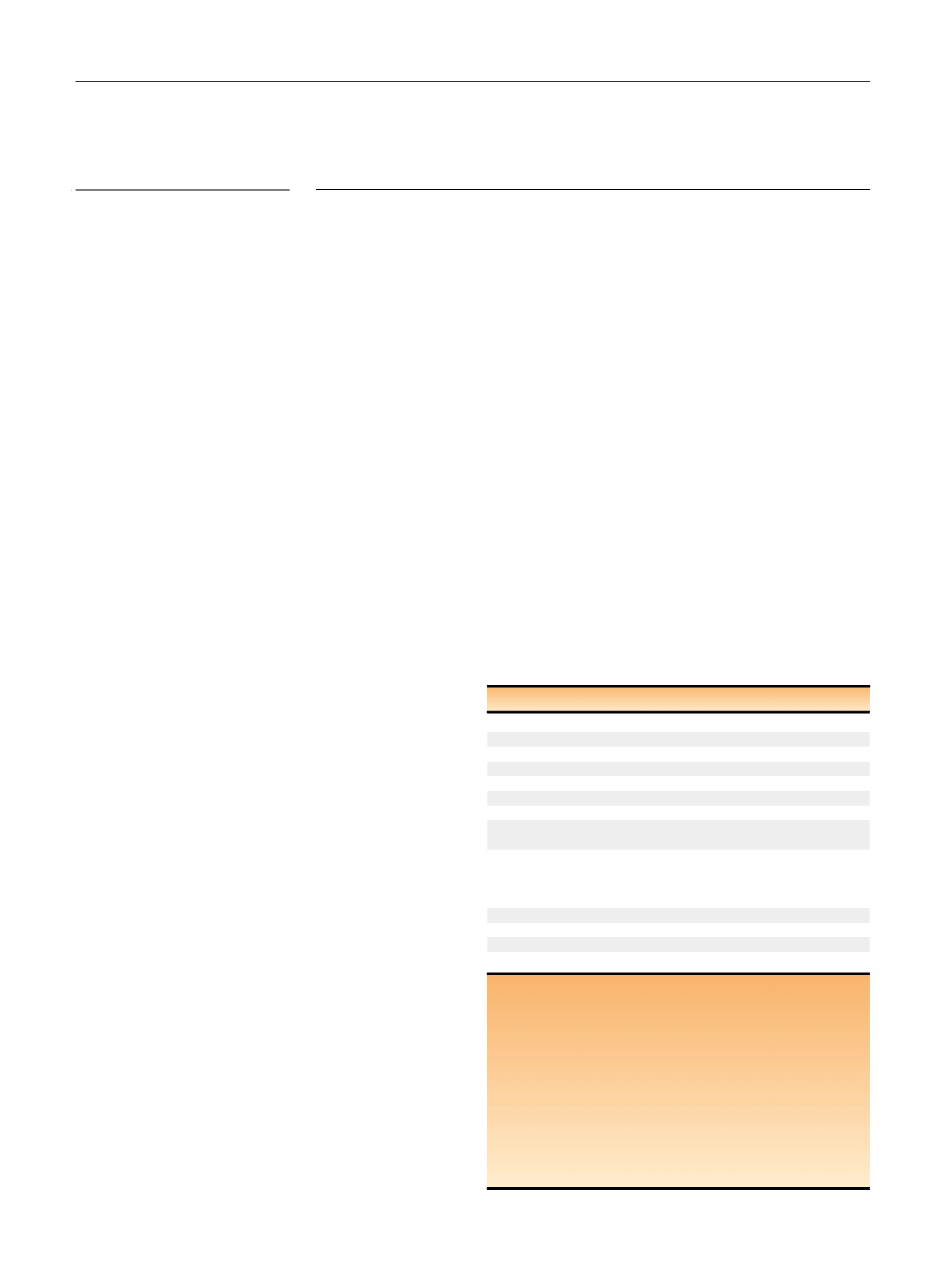
Table 1
–
Diagnostic strategies
Test
Strategies
MPMRI
First test
M1
–
M7; N1
–
N7
Second test after TRUSB
T5
–
T9; P5
–
P9
TRUSB
First test
T1
–
T9; P2
–
P9
Repeat TRUSB in men with no cancer detected
T2, T4
Repeat TRUSB in men with non-CS cancer detected T3, T4
Second test after MPMRI: MRI-targeted TRUSB,
in men with lesions visible at the MPMRI
M1
–
M7
Repeat MRI-targeted TRUSB in men with no
previous cancer or non-CS cancer at
fi
rst
MRI-targeted TRUSB, but with lesions visible
at MRI
M3
–
M7; T5
–
T9;
N3
–
N7
TPMB
First test
P1
Second test
P2
–
P4; N1
–
N4
Third test
P5
–
P9; N3
–
N7
MPMRI = multiparametric magnetic resonance imaging; TRUSB = transrectal
ultrasound-guided biopsy; TPMB = template prostate mapping biopsy;
CS = clinically signi
fi
cant. MRI-targeted TRUSB is a TRUSB informed by a
prior MPMRI. All TRUSB post-MPMRI are assumed to be MRI-targeted TRUSB.
Diagnostic strategies were labelled according to their test combination
fi
rst
(M1
–
M7, N1
–
N7, T1
–
T9, P1
–
P9), and then their biopsy TRUSB de
fi
nition (1 or
2), MPMRI de
fi
nition (1 or 2), and cut-off (2 to 5). T strategies start with
TRUSB, M strategies start with MPMRI, P strategies are the same as T
strategies, and N strategies are the same as M strategies but have TPMB as
the last biopsy. For example, strategy M1 125 refers to test combination M1,
in which all men were
fi
rst assessed using MPMRI de
fi
nition 2 and cut-off
5 and then followed up with biopsy de
fi
nition 1 for those with a suspicion of
CS cancer. See the Supplementary material, section 1, for full details on the
test sequences for each diagnostic strategy.
E U R O P E A N U R O L O GY 7 3 ( 2 0 18 ) 2 3
–
3 0
24
















