
eight patients (5%), stage could not be assigned. Tissue for
CGP was obtained from the kidney in 102 patients (60%)
and from metastatic sites in 67 patients (40%). Frequent
sites of metastasis included distant lymph nodes, soft
tissue, lung, and liver.
3.2.
Genomic characterization of advanced PRCC cases
An average of 2.4 mutations per tumor were detected. The
median tumor mutational burden (TMB) for all cases was
2.7 mutations/Mb and there was minimal variation in TMB
across subtypes, with 2.7 mutations/Mb representing the
median across type 1, type 2, and unclassified disease
( Table 1 ). In the overall cohort, the most frequent
alterations were in the
TERT
promoter (21%),
CDKN2A
(17%),
MET
(13%),
CDKN2B
(11%), and
FH
(11%)
( Fig. 1 A). One
pathogenic
FH
missense mutation was reported (R233H)
[17]; the remaining
FH
mutations were loss-of-function
truncation mutations. The median age was significantly
lower for patients with
FH
mutations compared to all PRCC
patients (37 vs 60 yr;
p
= 3 10
6
,
t
test, 2-tailed). In type
1 patients, the most commonly altered genes were
MET
(33%; 8 activating mutations, 5 amplifications at
>
6 copies),
TERT
(30%),
CDKN2A/B
(13%), and
EGFR
(8%;
1 activating mutation G598 V, 2 amplifications)
( Fig. 1B).
Out of the 13 type 1 PRCC cases with
MET
alterations, three
had a concurrent GA in
EGFR
(1 case with G598 V mutation,
1 with amplification) or
KRAS
(1 case with G12C). In type
2 patients, the most commonly altered genes were
CDKN2A/
B
(18%),
TERT
(18%),
NF2
(13%), and
FH
(13%);
MET
GAs
(5 mutations, 3 amplifications) were observed in 7% of type
2 patients
( Fig. 1 C).
Fig. 1 Dshows a pathway analysis
segregated by PRCC subtype. Alterations in SWI/SNF
complex genes were significantly associated with type
2 PRCC. Overall, frequent alterations were found in genes
coding for components of SWI/SNF complexes (26%),
chromatin modification (24%), and cell cycle regulation
(22%). RAS/RAF pathway (7%), PI3K/mTOR pathway (8%),
and DNA damage pathway (8%) alterations were observed,
although alterations in individual genes comprising these
pathways were less frequent.
Within the
MET
protooncogene, the preponderance of
alterations was found in the tyrosine kinase domain
( Fig. 2 ).
The most frequent
MET
alteration was H1094Y/L, seen in
three patients with type 1 disease and two patients with
type 2 disease.
MET
alterations found in more than one
patient include V1092I and F1200I.
Fig. 3highlights several of the key differences in GAs
between type 1 and type 2 PRCC in this cohort. A
significantly higher frequency of
MET
alteration was found
in type 1 versus type 2 disease (33% vs 7%;
p
= 0.0002).
Furthermore,
NF2
alterations were more frequent in type
2 versus type 1 disease (13% vs none;
p
= 0.02). Although not
statistically significant, a trend towards higher
TERT
promoter alterations in type 1 disease was observed (30%
vs 18%). By contrast, type 2 disease showed a trend towards
higher alterations in
SMARCB1
(9% vs 3%),
ARID1A
(10% vs
3%),
BAP1
(7% vs none),
SETD2
(9% vs 3%), and
PBRM1
(7% vs
none).
As noted in
Table 1, primary tumor (kidney) samples
were assessed more frequently than metastatic samples. A
slightly higher proportion of patients with type 2 disease
had metastatic samples for assessment (45%) compared to
patients with type 1 (33%) or unclassified disease (23%).
With this in mind, primary tumor specimens had a
significantly higher rate of alteration in
MET
(18% vs 6%;
p
= 0.03), while metastatic sites had a higher rate of
ARID1A
alterations (13% vs 4%;
p
= 0.04). Supplementary
Table 1highlights similar trends in
MET
and
ARID1A
alteration
frequencies between kidney and metastasis when segre-
gated by subtype (type 1 vs type 2).
A more detailed analysis of SWI/SNF pathway elements
is shown in
Fig. 4 .Overall, 26% of patients had alterations in
related genes, with the most frequent alterations noted in
SMARCB1
(8%),
ARID1A
(8%), and
PBRM1
(6%). The cumula-
tive frequency of SWI/SNF alterations was higher in type
2 than in type 1 disease (29% vs 11%;
p
= 0.027).
Pairwise analysis for co-occurrence/mutual exclusivity
was performed for the 12 most frequently mutated genes in
this study.
PBRM1/SETD2
mutation co-occurrence was
significant (
p
= 0.0001). At lower levels of significance,
BAP1/NF2
(
p
= 0.02) and
SETD2/BAP1
(
p
= 0.04) mutations
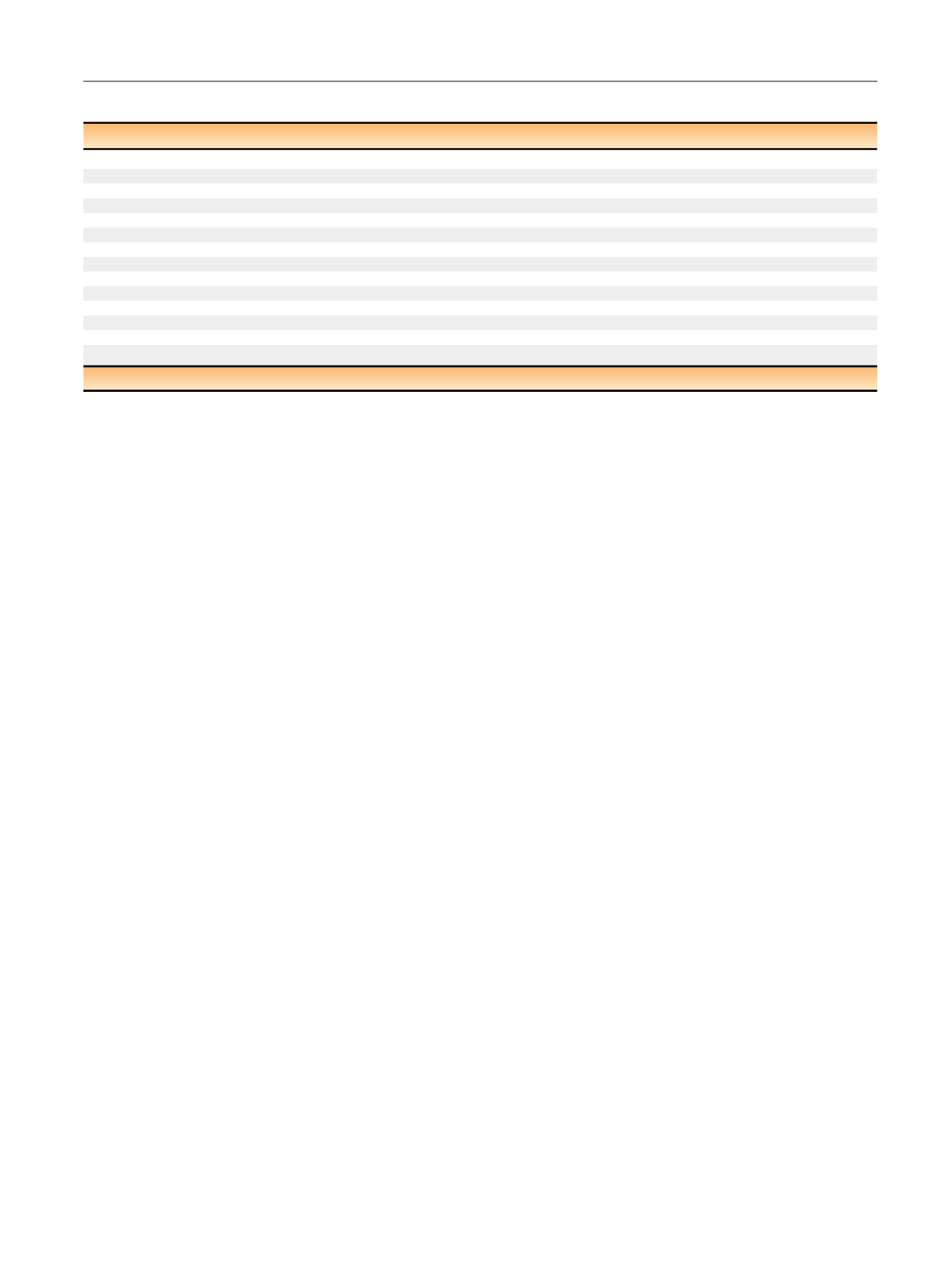
Table 1 – Patient characteristics
All
Type 1
Type 2
Unclassified
Patients (
n
)
169
39
108
22
Median age, yr (range)
60 (19–88)
60 (30–88)
59 (19–85)
61 (25–76)
Female,
n
(%)
40 (24)
10
26
4
Male,
n
(%)
129 (76)
29
82
18
Median TMB, mutations/Mb (range)
2.7 (0–13.5)
2.7 (0.9–9.0)
2.7 (0–13.5)
2.7 (0–8.1)
Sit of origin for sequenced sample (
n
)
Kidney
102
26
59
17
Metastasis
67
13
49
5
Clinical stage (
n
)
Stage I
14
5
7
2
Stage II
8
3
4
1
Stage III
36
9
22
5
Stage IV
103
20
70
13
Unknown
8
2
5
1
TMB = tumor mutational burden.
E U R O P E A N U R O L O G Y 7 3 ( 2 0 1 8 ) 7 1 – 7 8
73
















