
most common symptom is visible or nonvisible haematuria
(70
–
80%)
[1]. Flank pain occurs in approximately 20% of
cases, and a lumbar mass is present in approximately 10%
[1] .Systemic symptoms (including anorexia, weight loss,
malaise, fatigue, fever, night sweats, or cough) associated
with UTUC should prompt more rigorous metastatic
evaluation; they confer a worse prognosis
[1] .3.3.2.
Diagnosis
3.3.2.1. Imaging
3.3.2.1.1. Computed tomography urography.
Computed tomogra-
phy (CT) urography has the highest diagnostic accuracy of
the available imaging techniques
[1]. The sensitivity of CT
urography for UTUC is 0.67
–
1.0 and specificity is 0.93
–
0.99
[1,23].
Rapid acquisition of thin sections allows high-resolution
isotropic images that can be viewed in multiple planes to
assist with diagnosis without loss of resolution
[1]. Epithe-
lial
“
flat lesions
”
without mass effect or urothelial thicken-
ing are generally not visible with CT
[1] .The secondary sign of hydronephrosis is associated with
advanced disease and poor oncological outcome
[1,24,25] .The presence of enlarged lymph nodes is highly
predictive of metastases in UTUC
[1] .3.3.2.1.2. Magnetic resonance urography.
Magnetic resonance
(MR) urography is indicated in patients who cannot
undergo CT urography, usually when radiation or iodinated
contrast media are contraindicated
[1] .The sensitivity of
MR urography is 0.75 after contrast injection for tumours
<
2 cm
[1] .The use of MR urography with gadolinium-based
contrast media should be limited in patients with severe
renal impairment (
<
30 ml/min creatinine clearance), due
to the risk of nephrogenic systemic fibrosis.
CT urography is generally preferred to MR urography for
diagnosing and staging UTUC.
3.3.2.2. Cystoscopy and urinary cytology.
Positive urine cytology
is suggestive of UTUC when bladder cystoscopy is normal,
provided no CIS in the bladder or prostatic urethra has been
detected
[1] .Cytology is less sensitive for UTUC than bladder
tumours and should be performed
in situ
in the renal cavities
[26] .Retrograde ureteropyelography remains an option to
detect UTUCs
[1,23]. Urinary cytology of the renal cavities
and ureteral lumina is preferred before application of a
contrast agent for retrograde ureteropyelography because it
may cause deterioration of cytological specimens
[1,26].
The sensitivity of fluorescence
in situ
hybridisation
(FISH) for molecular abnormalities characteristic of UTUCs
parallels its performance in BCa. However, its use may be
limited by the preponderance of low-grade recurrent
disease in the population undergoing surveillance and
kidney-sparing therapy for UTUCs
[1] .Therefore, FISH has
limited value in the surveillance of UTUCs
[1] .3.3.2.3. Diagnostic ureteroscopy.
Flexible ureteroscopy is used
to visualise the ureter, renal pelvis, and collecting system
and biopsy suspicious lesions. Ureteroscopic biopsies
can determine tumour grade in 90% of cases with a low
false-negative rate, regardless of sample size
[27] .Under-
grading may occur following diagnostic biopsy, making
intensive follow-up necessary if kidney-sparing treatment
is chosen
[1]. Ureteroscopy also facilitates selective ureteral
sampling for cytology
in situ
[1,28]. Stage assessment using
ureteroscopic biopsy is notoriously difficult.
Flexible ureteroscopy is particularly useful in diagnostic
uncertainty, if kidney-sparing treatment is considered, or in
patients with a solitary kidney. Additional information can
be provided by ureteroscopy with or without biopsy.
Combining ureteroscopic biopsy grade, imaging findings
such as hydronephrosis, and urinary cytology may help in
the decision-making process between radical nephro-
ureterectomy (RNU) and kidney-sparing therapy
[1,28] .Technical developments in flexible ureteroscopes and
the use of novel imaging techniques improve visualisation
and diagnosis of flat lesions. Narrow-band imaging is a
promising technique, but results are preliminary
[1].
Recommendations are listed in
Table 2 .3.4.
Prognosis
3.4.1.
Prognostic factors
UTUCs that invade the muscle wall usually have a very poor
prognosis. The 5 yr specific survival is
<
50% for pT2/pT3 and
<
10% for pT4
[1,29]. The main prognostic factors are briefly
listed here.
Figure 2shows an exhaustive list.
3.4.1.1. Preoperative factors
3.4.1.1.1. Age and sex.
Gender is no longer considered an
independent prognostic factor influencing UTUC mortality
[1,9,29] .Older age at the time of RNU is independently
associated with decreased cancer-specific survival
[1,20](LE: 3). Many elderly patients can be cured with RNU
[1],
suggesting that age alone is an inadequate indicator of
outcome
[1]. Despite its association with survival, age alone
should not prevent a potentially curable approach.
3.4.1.1.2. Ethnicity.
One multicentre study did not show any
difference in outcome between races
[1], but population-
based studies have indicated that African-American patients
have worse outcomes than other ethnicities
[1](LE: 3).
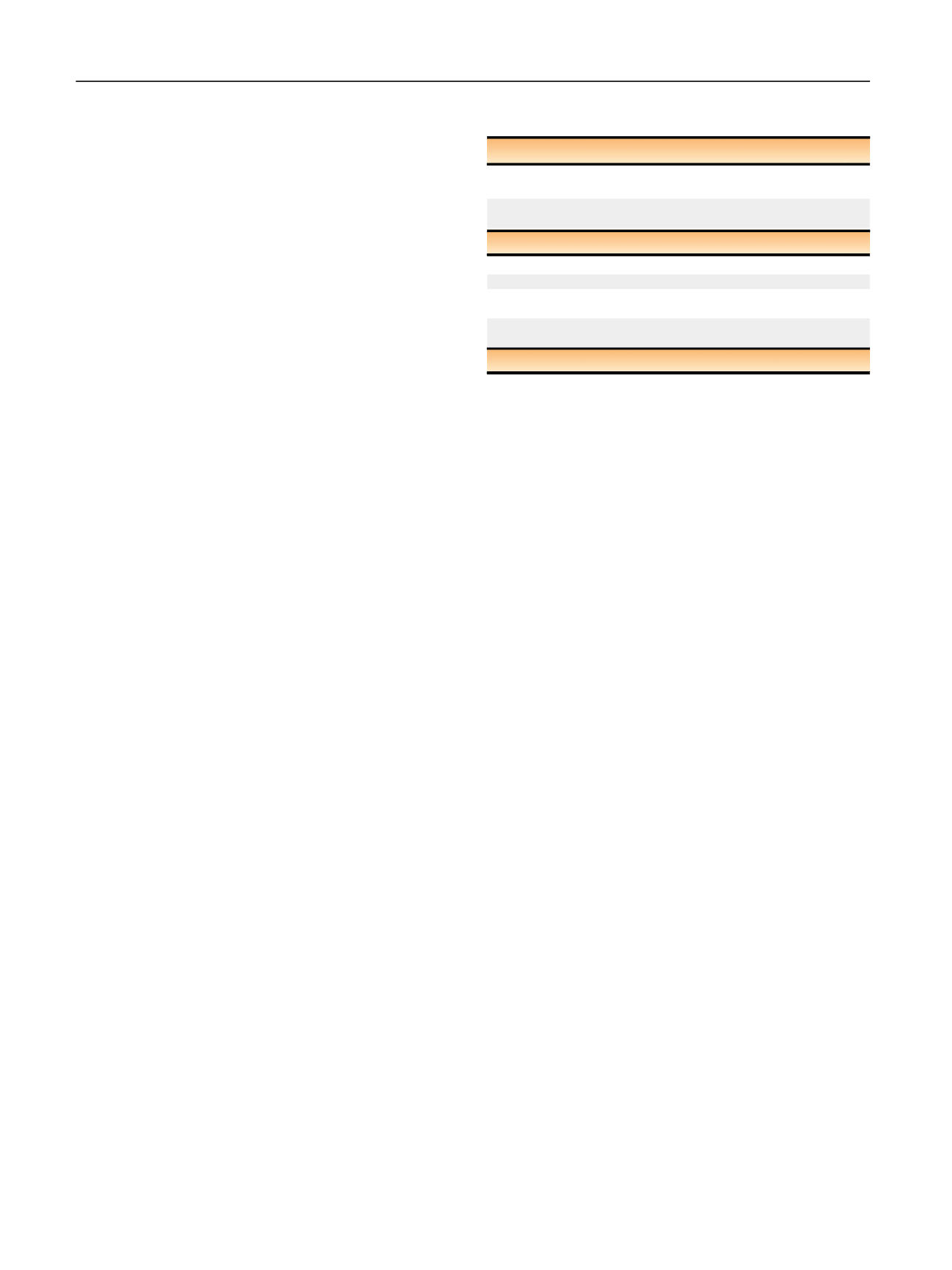
Table 2
–
Summary of evidence and guidelines for the diagnosis of
upper tract urothelial carcinoma
Summary of evidence
LE
The diagnosis of upper tract urothelial carcinoma depends
on computed tomography urography and ureteroscopy.
2
Selective urinary cytology has high sensitivity in high-grade
tumours including carcinoma
in situ
.
3
Recommendations
GR
Perform urinary cytology as part of a standard diagnostic workup.
A
Perform a cystoscopy to rule out concomitant bladder tumour.
A
Perform a computed tomography urography for upper tract
evaluation and for staging.
A
Use diagnostic ureteroscopy and biopsy in cases where additional
information will impact treatment decisions.
C
GR = grade of recommendation; LE = level of evidence.
E U R O P E A N U R O L O GY 7 3 ( 2 0 18 ) 111
–
1 2 2
114
















