
3.4.1.1.3. Tobacco consumption.
Being a smoker at diagnosis
increases the risk for disease recurrence and mortality
after RNU
[1,30]and recurrence within the bladder
[31](LE: 3). There is a close relationship between tobacco
consumption and prognosis; smoking cessation improves
cancer control.
3.4.1.1.4. Tumour location.
Initial location of the UTUC is a
prognostic factor in some studies
[1,32,33](LE: 3). After
adjustment for the effect of tumour stage, patients with
ureteral and/or multifocal tumours seem to have a worse
prognosis than renal pelvic tumours
[29,32 – 35] .3.4.1.1.5. Surgical delay.
A delay between diagnosis of an
invasive tumour and its removal may increase the risk of
disease progression. Once a decision regarding RNU has
been made, the procedure should be carried out within
12 wk when possible
[1,36 – 38](LE: 3).
3.4.1.1.6. Other.
The American Society of Anesthesiologists
score also significantly correlates with cancer-specific survival
after RNU
[39](LE: 3), but the Eastern Cooperative Oncology
Group performance status correlates only with overall
survival (OS)
[40]. Obesity and higher body mass index
adversely affect cancer-specific outcomes in UTUCs
[41](LE:
3). The pretreatment
–
derived neutrophil
–
lymphocyte ratio
also correlates with higher cancer-specific mortality
[42].
3.4.1.2. Postoperative factors
3.4.1.2.1. Tumour stage and grade.
The primary recognised
prognostic factors are tumour stage and grade
[1,28,29] .3.4.1.2.2. Lymph node involvement.
Lymph node metastases and
extranodal extension are powerful predictors of survival
outcomes in UTUC
[1]. Lymph node dissection (LND)
performed at the time of RNU allows for optimal tumour
staging
[1,43](LE: 3). Its curative role remains debated.
3.4.1.2.3. Lymphovascular invasion.
Lymphovascular invasion is
present in approximately 20% of UTUCs and is an indepen-
dent predictor of survival
[1]. Lymphovascular invasion
status should be specifically reported in the pathological
reports of all UTUC specimens
[1](LE: 3).
3.4.1.2.4. Surgical margins.
Positive soft tissue surgical margin
after RNU is a significant factor for developing disease
recurrence. Pathologists should look for and report positive
margins at the level of ureteral transection, bladder cuff, and
around the tumour if T
>
2
[44](LE: 3).
3.4.1.2.5. Pathological factors.
Extensive tumour necrosis (
>
10%
of the tumour area) is an independent prognostic predictor
in patients who undergo RNU
[1](LE: 3). The architecture of
UTUC is also a strong prognosticator with sessile growth
pattern being associated with worse outcome
[1](LE: 3).
Concomitant CIS in organ-confined UTUC and a history of
bladder CIS are associated with a higher risk of recurrence
and cancer-specific mortality
[1,45,46](LE: 3).
3.4.2.
Molecular markers
Several studies have investigated the prognostic impact of
markers related to cell adhesion (E-cadherin and CD24), cell
differentiation (Snail and epidermal growth factor receptor),
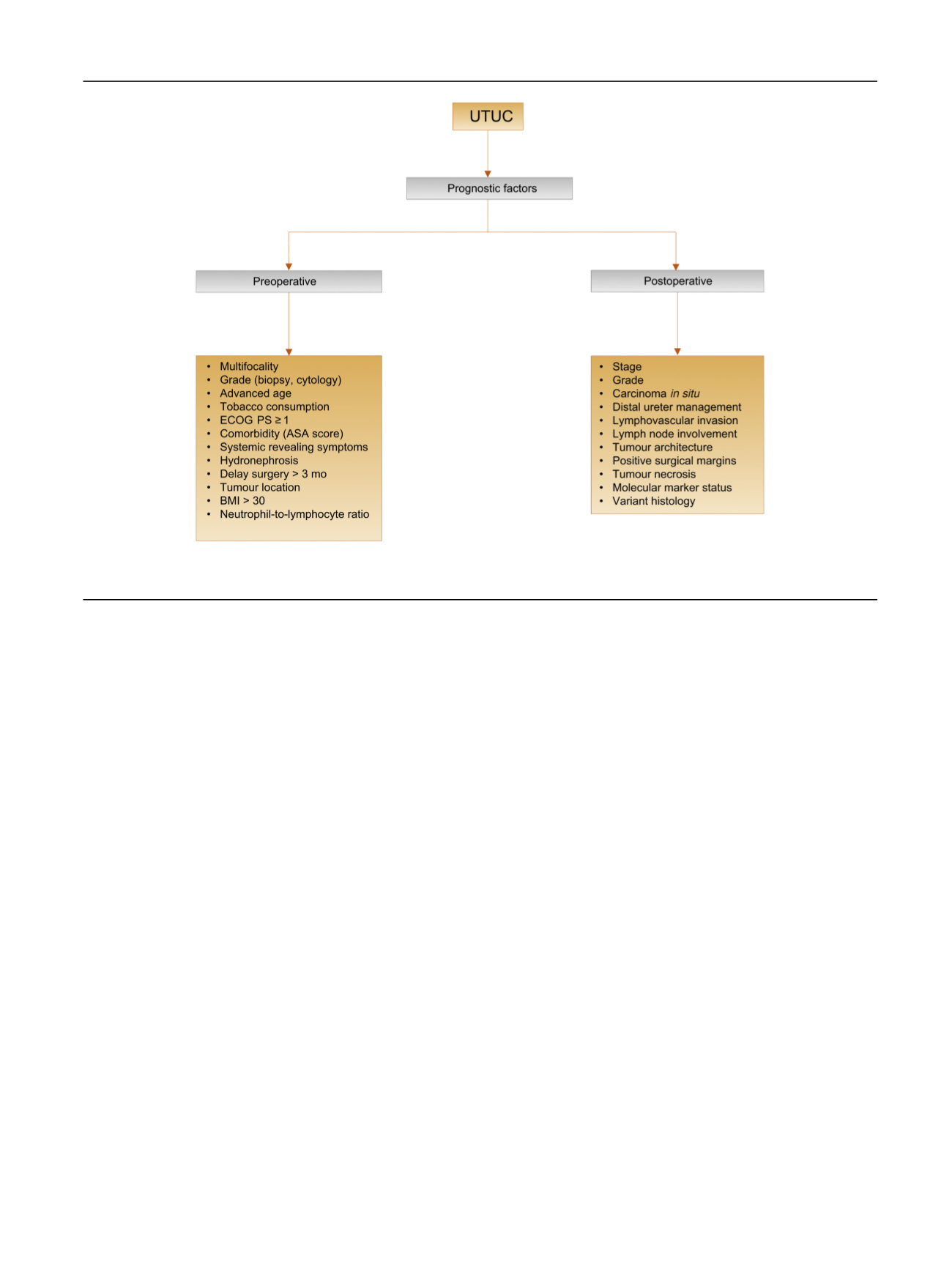
[(Fig._2)TD$FIG]
Fig. 2
–
Upper urinary tract urothelial carcinoma: prognostic factors. ASA = American Society of Anesthesiologists; BMI = body mass index; ECOG
PS = Eastern Cooperative Oncology Group performance status; UTUC = upper urinary tract urothelial carcinoma.
E U R O P E A N U R O L O GY 7 3 ( 2 0 18 ) 111
–
1 2 2
115
















