
manipulation of large tumours in a pneumoperitoneal
environment have been reported in few cases
[1] .Several precautions may lower the risk of tumour
spillage:
1. Avoid entering the urinary tract.
2. Avoid direct contact between instruments and the
tumour.
3. Laparoscopic RNU must take place in a closed system.
Avoid morcellation of the tumour and use an endobag for
tumour extraction.
4. The kidney and ureter must be removed
en bloc
with the
bladder cuff.
5. Invasive or large (T3/T4 and/or N+/M+) tumours are
contraindications for laparoscopic RNU until proved
otherwise.
Laparoscopic RNU is safe in experienced hands when
adhering to strict oncological principles. There is a tendency
towards equivalent oncological outcomes after laparoscopic
or open RNU
[1,62,63](LE: 3). Only one prospective
randomised study has shown that laparoscopic RNU is
not inferior to open RNU for noninvasive UTUC
[1](LE: 2).
Oncological outcomes after RNU have not changed signifi-
cantly over the past 3 decades despite staging and surgical
refinements
[64](LE: 3). A robot-assisted laparoscopic
approach can be considered, but solid data are still lacking
[65,66]3.5.1.2.2. Lymph node dissection.
The anatomic sites of
lymph node drainage have not yet been clearly defined.
The use of an LND template is likely to have a greater impact
on patient survival than the number of removed lymph
nodes
[1] .LND appears to be unnecessary in cases of TaT1 UTUC
because lymph node retrieval is reported in only 2.2% of T1
versus 16% of pT2
–
4 tumours
[1,67]. An increase in the
probability of lymph node
–
positive disease is related to pT
classification
[1]. However, it is likely that the true rate of
node-positive disease has been under-reported because
these data are retrospective.
Despite available studies evaluating templates to date, it
is not possible to standardise indication or extent of LND.
LND can be achieved following lymphatic drainage as
follows: LND on the side of the affected ureter, retroperito-
neal LND for higher ureteral tumour, and/or tumour of the
renal pelvis (ie, right side: border vena cava or right side of
the aorta; and left side: border aorta)
[1,43] .3.5.1.2.3. Adjuvant bladder instillation.
The rate of bladder
recurrence after RNU for UTUC is 22
–
47%. Two prospective
randomised trials have demonstrated that a single postop-
erative dose of intravesical chemotherapy (mitomycin C,
pirarubicin) soon after surgery (
<
72 h) reduces the risk of
bladder tumour recurrence within the 1st year post-RNU
[68,69](LE: 2) and in a meta-analysis
[70]. Management is
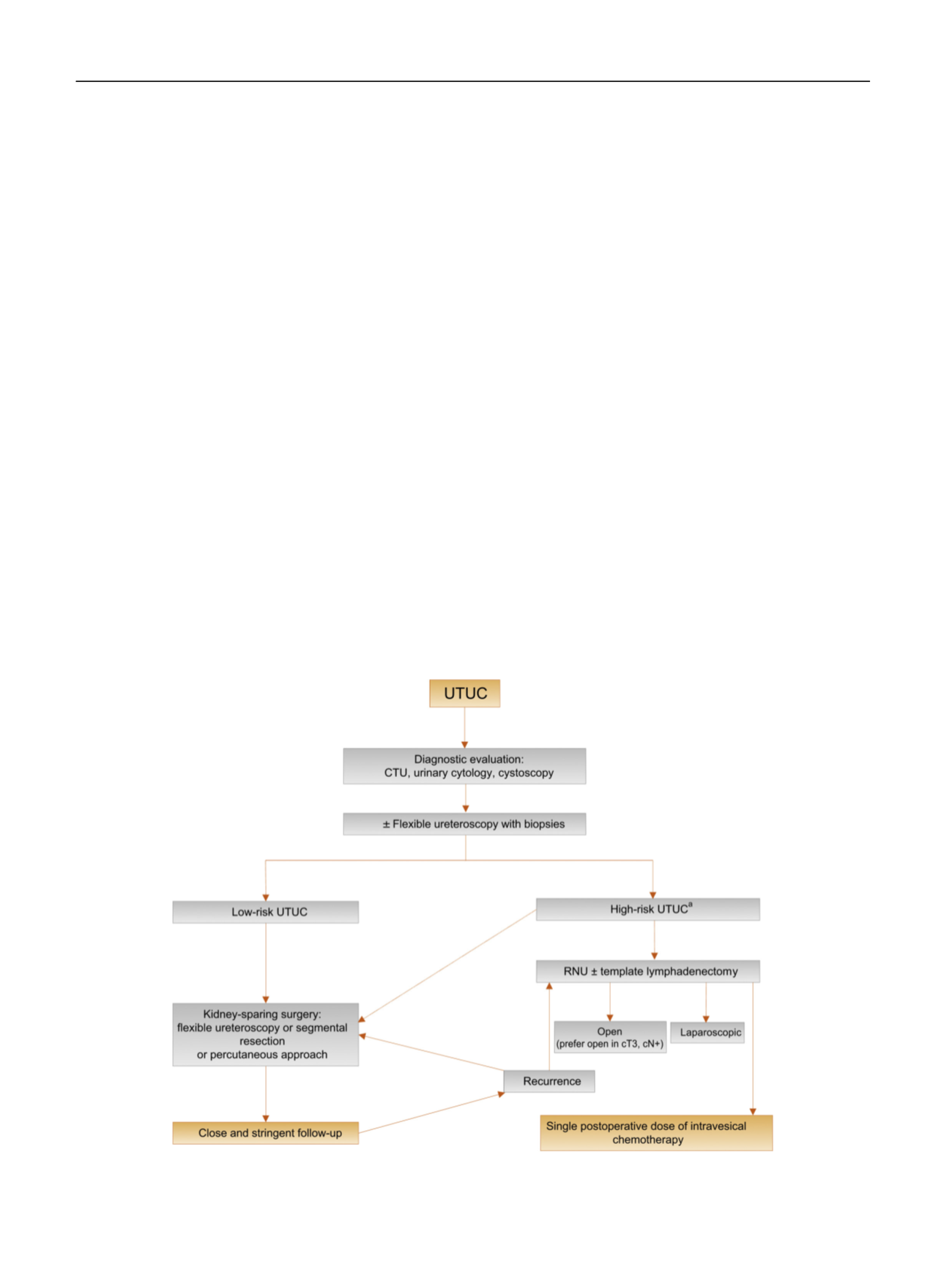
outlined in
Figures 4 and 5 .[(Fig._4)TD$FIG]
Fig. 4
–
Proposed flowchart for the management of upper urinary tract urothelial cell carcinoma. CTU = computed tomography urography; RNU = radical
nephroureterectomy; UTUC = upper urinary tract urothelial carcinoma.
a
In patients with solitary kidney, consider a more conservative approach.
E U R O P E A N U R O L O GY 7 3 ( 2 0 18 ) 111
–
1 2 2
118
















