
3.5.2.
Advanced disease
3.5.2.1. Radical nephroureterectomy.
There is no oncological
benefit for RNU alone in patients with metastatic UTUC
except for palliative considerations
[1,8](LE: 3).
3.5.2.2. Systemic chemotherapy.
Extrapolating from the BCa
literature and small, single-centre UTUC studies, plati-
num-based combination chemotherapy is expected to be
efficacious in UTUC. However, there are currently insuffi-
cient data upon which to base recommendations.
There are several platinum-based regimens
[1], but not
all patients can receive adjuvant chemotherapy because of
comorbidities and impaired renal function after radical
surgery. Chemotherapy-related toxicity, particularly neph-
rotoxicity due to platinum derivatives, may significantly
reduce survival in patients with postoperative renal
dysfunction
[1].
There were no adverse effects of neoadjuvant chemo-
therapy for UTUC
[71] ,although survival data need to
mature and longer follow-up is awaited. In a select cohort of
patients fit to receive systemic chemotherapy for metastatic
UTUC, there was an OS benefit to combine chemotherapy
and RNU versus chemotherapy alone
[72] .After a recent comprehensive search of studies examin-
ing the role of perioperative chemotherapy for UTUC, there
appears to be an OS and disease-free survival benefit for
cisplatin-based adjuvant chemotherapy
[73](LE: 3).
A recent study has assessed a clear OS benefit in patients
who received adjuvant chemotherapy versus observation
after RNU for pT3/T4 and/or pN+ UTUC
[74](LE: 3).
3.5.2.3. Radiotherapy.
Radiotherapy is no longer relevant,
either alone or as an adjunct to chemotherapy
[1](LE: 3).
3.5.3.
Follow-up
The risk of recurrence and death evolves during the follow-
up period after surgery
[75] .Stringent follow-up
( Table 5) is
mandatory to detect metachronous bladder tumours
(probability increases over time
[76] ), local recurrence,
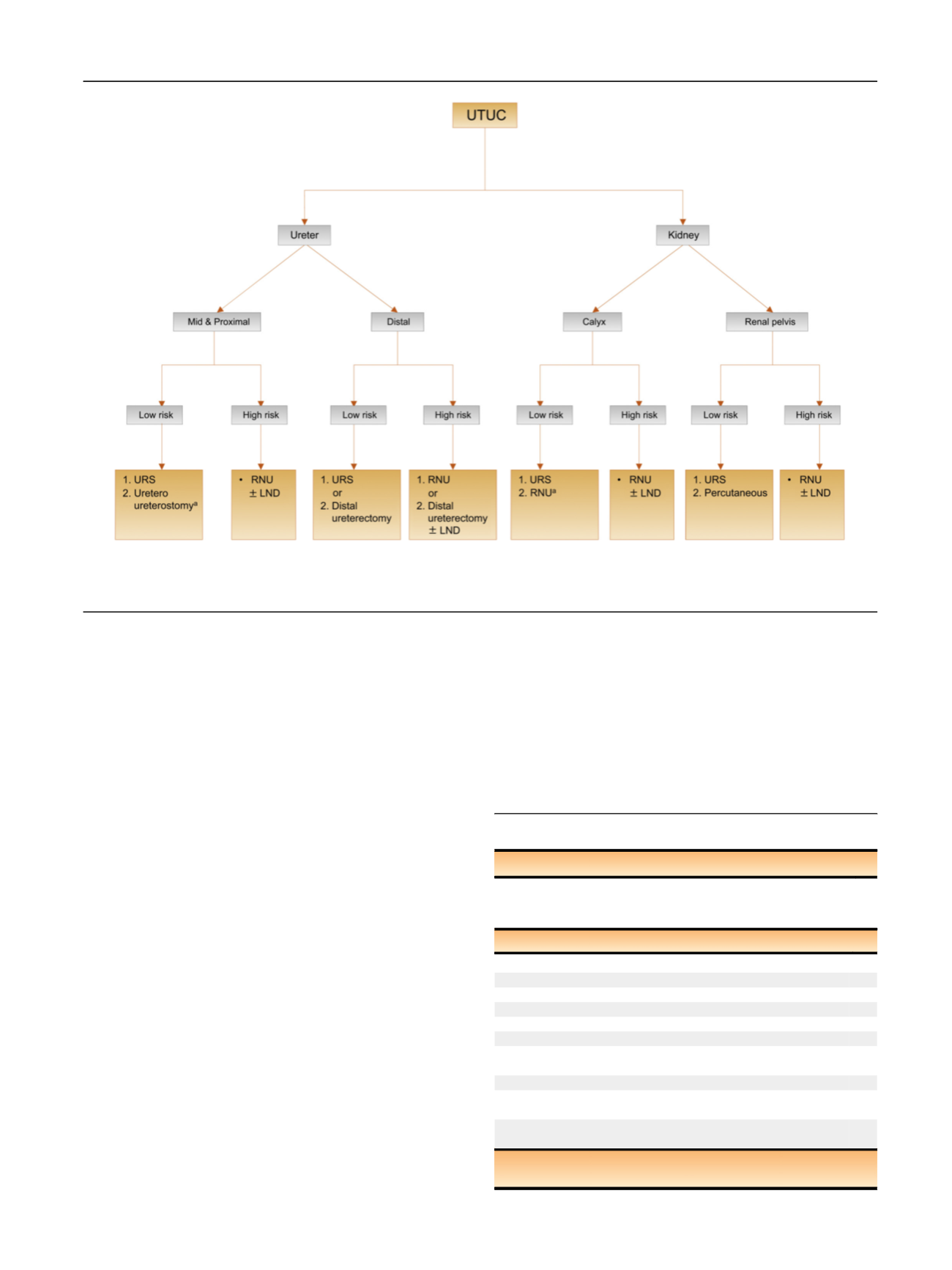
[(Fig._5)TD$FIG]
Fig. 5
–
Surgical treatment according to location and risk status. 1 = first treatment option; 2 = secondary treatment option. LND = lymph node
dissection; RNU = radical nephroureterectomy; URS = ureteroscopy; UTUC = upper urinary tract urothelial carcinoma.
a
In case not amendable to
endoscopic management.
Table 6
–
Summary of evidence and follow-up of UTUC
Summary of evidence
LE
Follow-up is more frequent and stricter in patients who
have undergone kidney-sparing treatment compared to radical
nephroureterectomy.
3
Recommendations
GR
After radical nephroureterectomy,
>
5 yr
Noninvasive tumour
Perform cystoscopy/urinary cytology at 3 mo, and then annually. C
Perform computed tomography urography every year.
C
Invasive tumour
Perform cystoscopy/urinary cytology at 3 mo, and then annually. C
Perform computed tomography urography every 6 mo for
2 yr, and then annually.
C
After kidney-sparing management,
>
5 yr
Perform urinary cytology and computed tomography urography
at 3 and 6 mo, and then annually.
C
Perform cystoscopy, ureteroscopy, and cytology
in situ
at 3 and
6 mo, and then every 6 mo for 2 yr, and then annually.
C
GR = grade of recommendation; LE = level of evidence; UTUC = upper
urinary tract urothelial carcinoma.
E U R O P E A N U R O L O GY 7 3 ( 2 0 18 ) 111
–
1 2 2
119
















