
of AP and BCR
[7,8] ,and has now been shown to be a strong,
independent predictor of key late end points, including
metastases and PCD, and to improve risk stratification over
clinicopathological features alone. A major strength of this
study is that it was performed in a cohort of contemporane-
ously and uniformly treated patients in a large community-
based healthcare network, thus providing a representative
“
real-world
”
mix of patients and clinical outcomes.
Now, a number of molecular tests are available at the
time of biopsy and/or surgery that may improve risk
stratification and assist with treatment decisions in men
with clinically localized PCa. Since none of the assays have
been compared with each other in prospective head-to-
head clinical studies, it is currently not possible to directly
know the relative value, although all have found associa-
tions between the assay and metastasis or PCD
[20 – 23].
It was noteworthy that no patients in this study with
NCCN very low
–
, low-, and intermediate-risk disease
(
n
= 31) and a GPS of
<
20 suffered a late event (metastases
or PCD). This finding has been corroborated in data from
prior studies of GPS
[24], suggesting that this subset of
patients is at a very low risk of harboring lethal PCa and is
particularly suitable to be followed with AS rather than
immediate definitive therapy.
Another strength of this study is that the cohort
comprises the full spectrum of clinical risk from very low
–
to high-risk disease. Prior GPS clinical validation studies
were limited to patients with very low
–
to favorable
intermediate
–
risk disease, and supported the utility of the
assay for patients considering AS
[7,8]. It is notable that
NCCN intermediate-risk patients with GPS
>
40 had a 5-yr
risk of distant metastases, which was similar to that of
NCCN high-risk patients, suggesting that this subset of
clinically intermediate
–
risk patients may benefit from
intensified treatment. These findings are consistent with
prior observations in other cohorts that intermediate-risk
patients with GPS
>
40 had similar risks of BCR and clinical
recurrence to high-risk patients (unpublished data), and
will require further confirmation.
It is important to note that all patients in the cohort had
undergone definitive therapy with RP, and thus a limitation
of the study is that it did not assess outcomes in patients
managed with AS or radiation therapy (RT). Thus, the 10-yr
risk of PCD and metastasis may be higher than that
estimated by the risk profiles from this study if a patient
was initially managed with AS or RT. While it is unknown
howGPS would perform inmenwhowere managedwith AS
or RT, results from previous randomized clinical trials
comparing conservative management with immediate
treatment suggest that these risks are unlikely to be
significantly higher
[25 – 27] .Studies of GPS in the setting
of AS and RT are underway in independent cohorts.
An additional limitation was a patient population that
spanned from 1995 to 2010. While it is essentially
impossible to conduct a truly contemporary study, given
the long natural history of the disease, changes in clinical
care that have occurred during this period, in particular,
changes in biopsy schemes from sextant biopsies to
extended ( 12 cores) biopsies, and the use of magnetic
resonance imaging
–
guided biopsy need to be kept in mind
when interpreting these results. Nonetheless, we found that
GPS was a significant predictor of outcome within the
subset of more contemporary patients who underwent
extended ( 12 cores) biopsy schemes.
5.
Conclusions
The 17-gene GPS assay independently predicted PCD,
distant metastasis, and BCR in a cohort of community-
managed, surgically treated men with adenocarcinoma of
the prostate, and may be a useful adjunct in risk
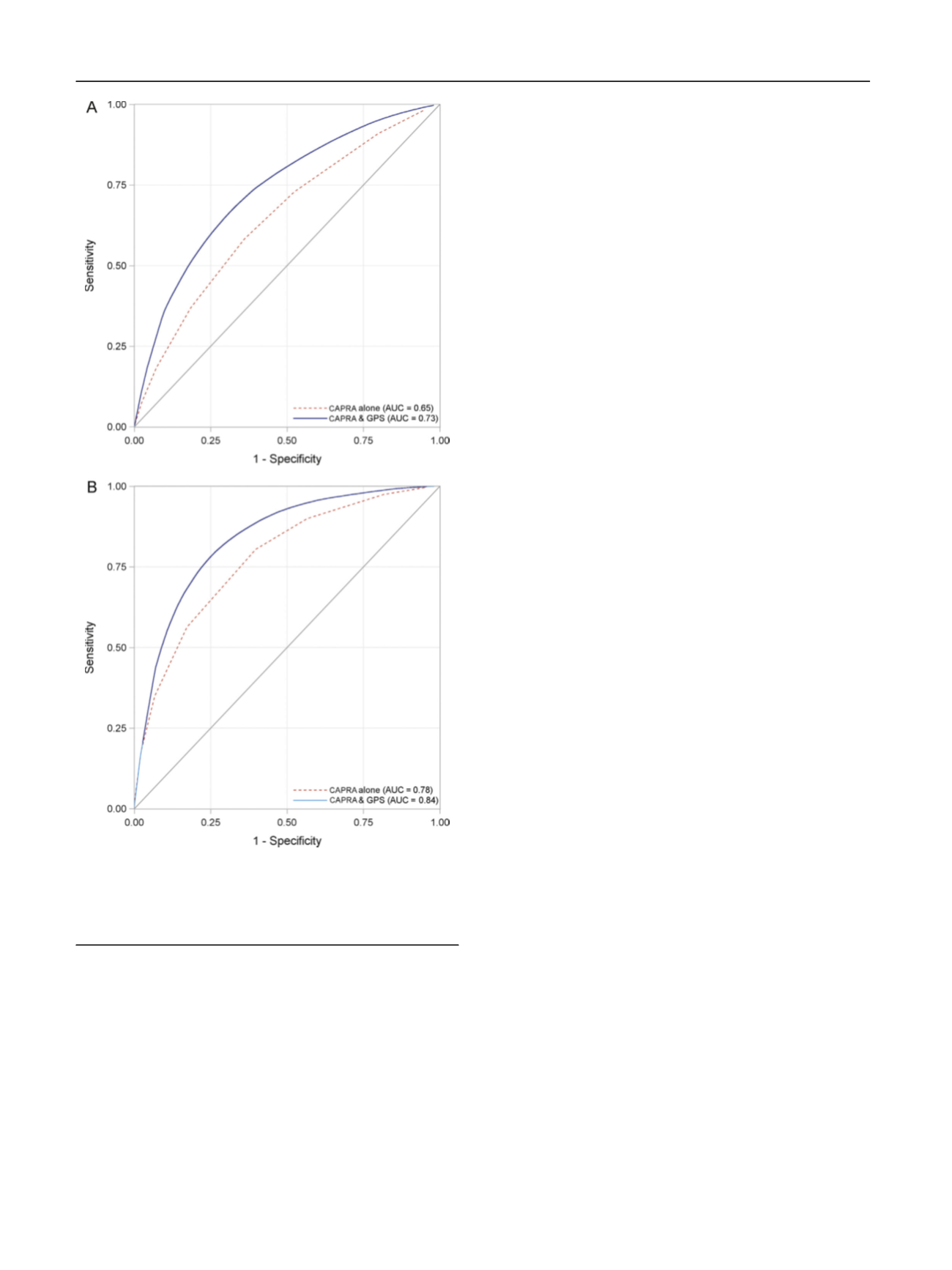
[(Fig._4)TD$FIG]
Fig. 4
–
Clinical utility: GPS improves prediction accuracy of 10-yr risk
of (A) metastasis and (B) PCD with higher AUCs over NCCN risk group
alone. AUC = area under the curve; CAPRA = Cancer of the Prostate Risk
Assessment; GPS = Genomic Prostate Score; NCCN = National
Comprehensive Cancer Network; PCD = prostate cancer death.
E U R O P E A N U R O L O GY 7 3 ( 2 0 18 ) 1 2 9
–
13 8
136
















