
the 2005 International Society of Urological Pathology
consensus guideline update.
Median GPS increased with higher NCCN risk (
p
<
0.001),
although there was a broad and substantially overlapping
range of GPS values for each clinical risk group. Median GPS
values were similar in racial groups and were not
statistically significant
( Fig. 2).
3.2.
GPS as a predictor of distant metastases
The 259 evaluable patients included 79 (weighted propor-
tion = 9%) with distant metastases and 180 with nonme-
tastases. In univariable analysis, GPS was significantly
predictive of time to metastases (HR/20 GPS units = 2.75;
95% CI 1.63
–
4.63;
p
= 0.0002). Central biopsy GS and clinical
risk group were significantly associated with time to
metastases (
p
<
0.05) in univariable analysis, but race,
clinical T stage, percent of positive biopsy cores, and
diagnostic PSAwere not. The lack of a significant association
of these latter factors with metastasis may reflect insuffi-
cient statistical power for those factors. In multivariable
analyses with GPS and NCCN risk group, GPS remained
significant (HR/20 units = 2.34;
p
<
0.001; 95% CI 1.42
–
3.86). GPS was also significantly associated with time to
metastases after adjusting for American Urological Associ-
ation (AUA) and Cancer of the Prostate Risk Assessment
(CAPRA) scores with similar HRs (
p
<
0.001;
Table 2). The
Cox PH models for metastases met linearity and PH
assumptions.
3.3.
GPS as a predictor of PCD
The 259 evaluable patients included 64 PCD (weighted
proportion = 2%) and 195 non-PCD patients. In univariable
analysis, GPS was strongly associated with time to PCD
(HR/20 units = 3.23;
p
<
0.001; 95% CI 1.84
–
5.65). In
univariable analysis, age, central biopsy GS, percent of
positive core, diagnostic PSA, PSA density, and clinical risk
groups were significantly associated with PCD, but race and
clinical T stage were not. The association of GPS with time
to PCD remained significant in multivariable analysis after
adjusting for NCCN (HR/20 units = 2.69;
p
<
0.001; 95% CI
1.50
–
4.82), and for AUA and CAPRA with similar HRs (both
p
<
0.001;
Table 2).
In the Cox PH model for PCD, the linearity assumption
was valid, but there was significant nonproportionality of
hazards (
p
= 0.0008). The HR of 3.23/20 GPS units repre-
sented an average over the duration of follow-up. The
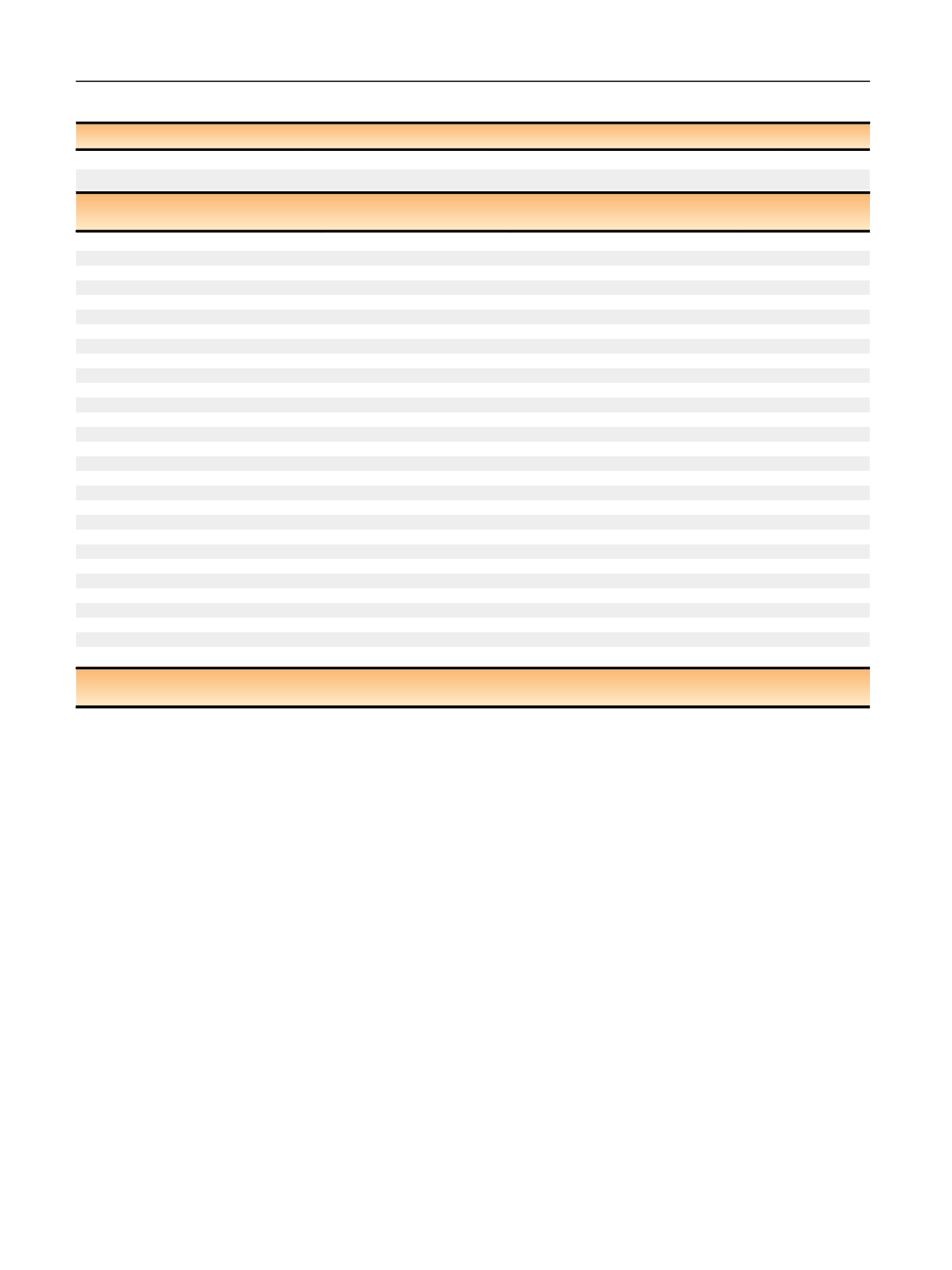
Table 1
–
Demographic and clinical characteristics of final evaluable cohort (
n
= 259)
Characteristic
Statistics
Study cohort (weighted statistics)
KPNCDOR total
Age (yr)
Median (IQR)
61 (57
–
65)
61 (56
–
66)
PSA density (ng/ml/cc)
Median (IQR)
0.18 (0.12
–
0.26)
NA
Characteristic
Values
Number of patients in the
study cohort (weighted %)
Number of patients in
KPNCDOR total (%)
Race/ethnicity
White non-Hispanic
201 (79.0%)
4304 (69.6%)
African American
26 (11.0%)
724 (11.7%)
Other
32 (10.0%)
1156 (18.7%)
PSA (ng/ml)
0
–
4
24 (9.5%)
493 (8.0%)
4.1
–
10
159 (70.1%)
4510 (72.9%)
10.1
75 (20.4%)
1042 (16.9%)
Clinical T stage
T1
67 (24.9%)
1550 (25.1%)
T2
189 (74.6%)
4562 (73.8%)
T3
2 (0.4%)
17 (0.3%)
Original biopsy Gleason score
3 + 3
117 (62.3%)
3350 (58.5%)
3 + 4
58 (20.7%)
2097 (36.6%)
4 + 3
30 (8.7%)
4 + 4
26 (3.8%)
196 (3.4%)
Any pattern 5
20 (4.5%)
81 (1.4%)
Central biopsy Gleason score
3 + 3
69 (37.6%)
NA
3 + 4
113 (45.5%)
NA
4 + 3
42 (11.4%)
NA
4 + 4
12 (2.7%)
NA
Any pattern 5
23 (2.8%)
NA
NCCN risk group
Very low
5 (3.0%)
NA
Low
35 (20.6%)
NA
Intermediate
160 (67.1%)
NA
High
57 (9.3%)
NA
CAPRA score
0
–
2
85 (46.9%)
NA
3
–
5
130 (46.3%)
NA
6
–
10
42 (6.9%)
NA
Treatment year
1995
–
2000
100 (24.3%)
1532 (25.9%)
2001
–
2005
64 (27.5%)
1581 (26.7%)
2006
–
2010
95 (48.2%)
2798 (47.3%)
CAPRA = Cancer of the Prostate Risk Assessment; IQR = interquartile range; KPNCDOR = Kaiser Permanente Northern California Division of Research; NA = not
available; PSA = prostate-speci
fi
c antigen.
E U R O P E A N U R O L O GY 7 3 ( 2 0 18 ) 1 2 9
–
13 8
132
















