
Twelve trials evaluate the impact of age on OS after RC in
multivariate analysis
( Table 2)
[5,14–17,19–25]. All but two
[16,19]confirm that increasing age is significantly associ-
ated with worse survival for patients aged
>
70 yr compared
with patients
<
70 yr old with reported hazard ratios
between 1.34 (95% confidence interval [CI]: 1.03–1.74) and
1.46 (95% CI: 1.08–1.97). Obviously, the risk of dying further
increases for patients aged
>
80 yr when compared with
patients
<
70 yr (reported hazard ratio between 1.63 [95%
CI: 1.06–2.53] and 3.22 [95% CI: 2.6–3.98]). For patients
treated with external beam radiotherapy, two trials
reported similar hazard ratios with favourable outcome
for younger people
[24,25].
3.2.
CSS
CSS estimates for different age groups are presented in
Table 3. As for OS, CSS worsens with age when patients are
treated with RC as is demonstrated in eight out of 12 articles
[6,8,9,11,15–17,26–30]. Studies evaluating the impact of age
on CSS in multivariate analysis are not able to demonstrate
worse outcome for patients aged
>
70 yr compared with
patients aged
<
60 yr
( Table 4 ) [15–17,19,21,23,28,31].
However, age
>
80 yr remains a significant predictor for
CSS with hazard ratios ranging from 1.56 to 2.54.
Only two articles reported on CSS after combined
chemoradiotherapy
[32,33]. A pooled analysis of patients
treated with selective bladder-preserving combined mo-
dality therapy, enrolled in different Radiation Therapy
Oncology Group protocols, did not show worsening of
outcome with age with 5-yr CSS of 70% and 71% for patients
aged 75 yr and older, respectively
[32].
3.3.
Morbidity
The incidence of morbidity after RC for MIBC in old versus
young patients is presented in
Fig. 2and Supplementary
Table 3
[7,8,11,12,15,16,18,27,30,34–39,41] .Overall peri-
operative mortality and early mortality is increased in older
patients (absolute incidence of POM: 1–6% for patients aged
<
70 yr vs 0–15% for patients aged
>
70 yr). Multivariate
analysis confirms that POM is significantly increased with
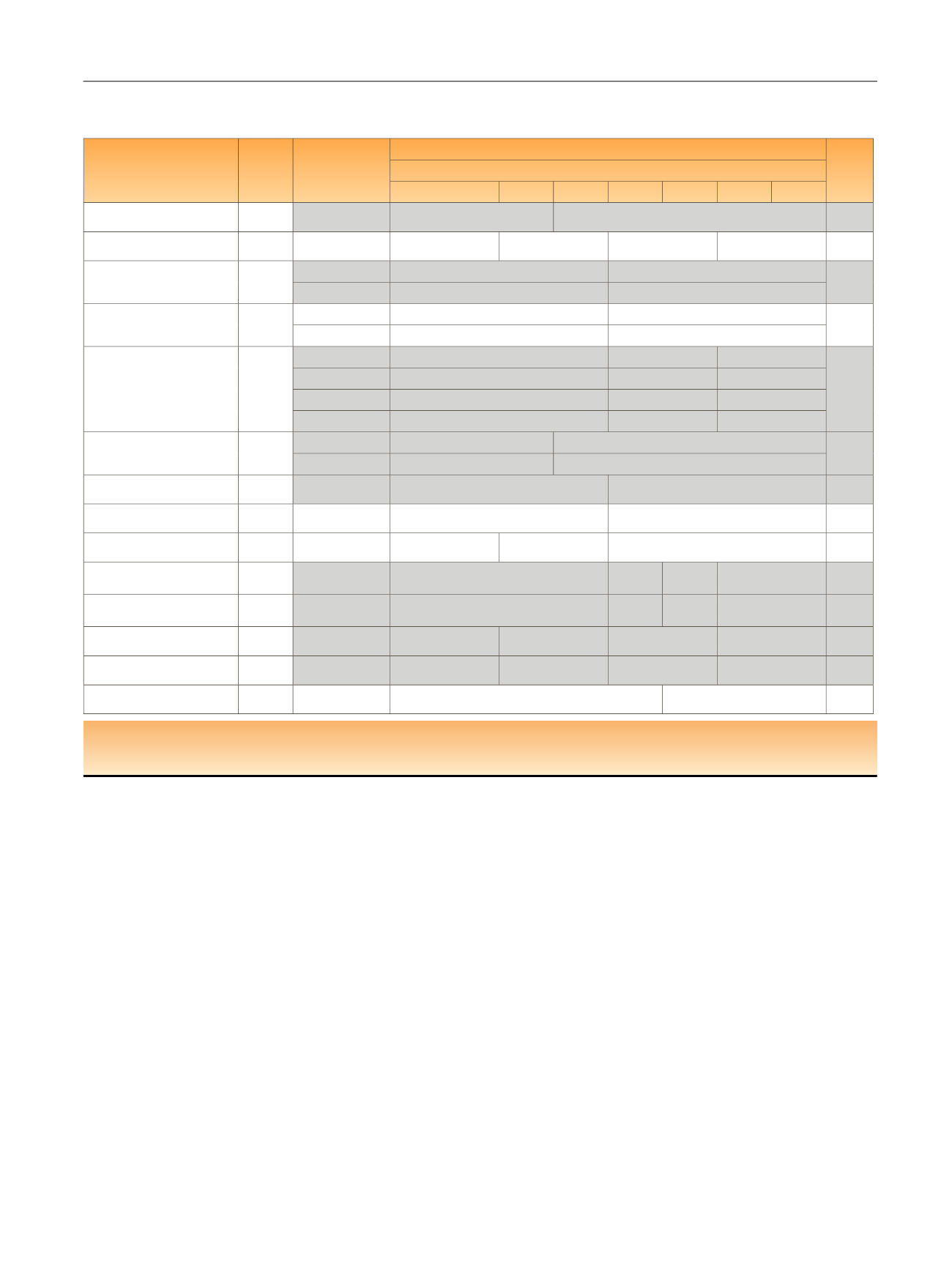
Table 1 – Reported estimates of overall survival rates per age group and per study. The studies in grey represent the studies where a
significant difference was observed between younger and older patients
Author
N
Reported
measure unit
Trials with radical cystectomy
p
value
Overall survival
80–84
75–79
70–74
65–69
60–64
<60
≥85
Hafron et al [5] 2005
288
Median survival
(mo)
70.4 (
N
= 132)
38.9 (
N
= 156)
<0.001
Horovitz et al [6] 2012
70% (
3 yr
605
N
= 165)
67% (
N
= 192)
66% (
N
= 201)
58% (
N
= 47)
0.4
Figueroa et al [7] 1997
1168
3 yr
68% (
N
= 762)
60% (
N
= 404)
0.001
5 yr
63%
53%
390
Rink et al [8] 2011
70% (
N
= 265)
2 yr
(
N
= 125)
68%
0.16
41%
57%
ry5
Liberman et al [9] 2011
a
12 722
1 yr
85% (
N
= 6803)
76% (
N
= 4480)
64% (
N
= 1439)
<0.001
2 yr
71%
60%
46%
5 yr
54%
42%
23%
10 yr
42%
25%
10%
Pollack et al [10] 1994
b
338
5 yr
47% (
N
= 204)
41% (
N
= 134)
0.03
10 yr
36%
25%
Guillotreau et al [11] 2012
146
5 yr
87% (
N
= 72)
75% (
N
= 74)
0.03
Fontana et al [12] 2015
50% (
N
5 yr
180
(
N
= 77)
50%
= 103)
NS
Böstrum et al [13] 2009
52% (
N
= 62)
10 yr
248
50% (
N
= 98)
39% (
N
= 64)
0.159
Nisjiyama et al [14] 2004
1113
5 yr
71% (
N
= 691)
65% (
N
=
268)
60% (
N
=
110)
56% (
N
= 62)
0.001
Leveridge et al [15] 2015
3320
5 yr
40% (
N
= 1362)
34% (
N
=
674)
28% (
N
=
627)
23% (
N
= 657)
<0.001
Fairey et al [16] 2012
2263
5 yr
62% (
N
= 557)
60% (
N
= 679)
55% (
N
= 846)
36% (
N
= 181)
<0.0001
Patel et al [17] 2015
804
5 yr
60% (
N
= 150)
45% (
N
= 245)
41% (
N
= 339)
30% (
N
= 70)
<0.001
Hara et al [18] 2016
(
N
= 162)
63%
ry5
254
(
N
= 92)
62%
0.983
a
Studies based on Surveillance, Epidemiology, and End Results registries.
b
Trial on preoperative radiotherapy.
NS = not significant.
E U R O P E A N U R O L O G Y 7 3 ( 2 0 1 8 ) 4 0 – 5 0
43
















