
discouraged, but the G8 seems the most robust
[55]. Pro-
spective studies evaluating the impact of using GAs on the
decision-making process are needed.
Not only OS but also CSS after RC is worse for older
patients, implying that age alone is not responsible for
worse outcome.
Besides differences in health status, a poorer outcome in
elderly patients might be explained by the observation that
these patients often receive a suboptimal
curative
treat-
ment. This, despite compelling evidence that, even in
patients aged 80 yr, an aggressive approach improves
survival
[56] .There is Level 1 evidence that neoadjuvant
chemotherapy improves survival significantly
[57]. Poor
performance status and impaired kidney function in elderly
are contraindications for platinum-based chemotherapy
and can discourage physicians to use perioperative chemo-
therapy
[15,16,58,59]or lead to dosage reduction
[60]. Data
do, however, indicate that neoadjuvant chemotherapy can
be administrated safely and with comparable clinical
outcome to patients aged
<
70 yr in appropriately selected
elderly patients
[61]. Information of administration of
perioperative chemotherapy in the selected articles was
limited.
Although it is recommended to perform a RC with a
pelvic lymph node dissection, the place of an extended
lymph node dissection remains debatable, particularly in
elderly patients
[62]. Nevertheless, several articles have
suggested a correlation between extent of pelvic lymph
node dissection and outcome
[63,64], in both patients aged
<
80 yr and octogenarians
[58] .In practice, an extended
pelvic lymph node dissection is often omitted in elderly
patients in order to limit operative time and reduce the risk
of postsurgical complications
[15,58].
Also, the type of urinary diversion differs between age
groups. Therefore, will older patients more likely receive
incontinent urinary diversions such as an ileal conduit
(6,16,27,34–36,42,45). Whether the type of diversion on its
own has a major impact on clinical outcome is doubtful
[35,65]. However, this could suggest that elderly patients are
diagnosed at more advanced stages
[8,16,21]as patients
with advanced clinical stage are more likely to receive
incontinent urinary diversions
[44]. Only eight articles
included in this systematic review reported the tumor stage
per age group. Four articles reported more advanced tumor
stage at presentation in elderly patients with inferior CSS
and/or OS for elderly patients in three of them
[8,16,27]. Four
articles
[6,11,18,37]did not found differences in stage
distribution between younger and older patients. Similar OS
between both groups was reported in two of them
[6,18]. In
contrast to OS, CSS was not worse for elderly patients in the
publication of Guillotreau et al
[11]. With similar tumor
stage at presentation the complication rate appears compa-
rable between younger and older patients
[37].
A major concern when treating older patients with
radical cystectomy is POM. Good patient evaluation is
crucial to improve patient survival. Not surprisingly, older
patients have a poorer American Society of Anaesthesiol-
ogists physical status classification
[66]. Despite improve-
ments in perioperative care resulting in a significant
reduction of POM, POM remains more prevalent in
septuagenarians with a 2- to 6-fold increased risk compared
with patients
<
70 yr old. Perioperative mortality has
decreased significantly with time in high-volume and
moderate-volume centres pointing out the importance of
referring patients, certainly those who are most vulnerable
of dying from the procedure, to those centres
[17].
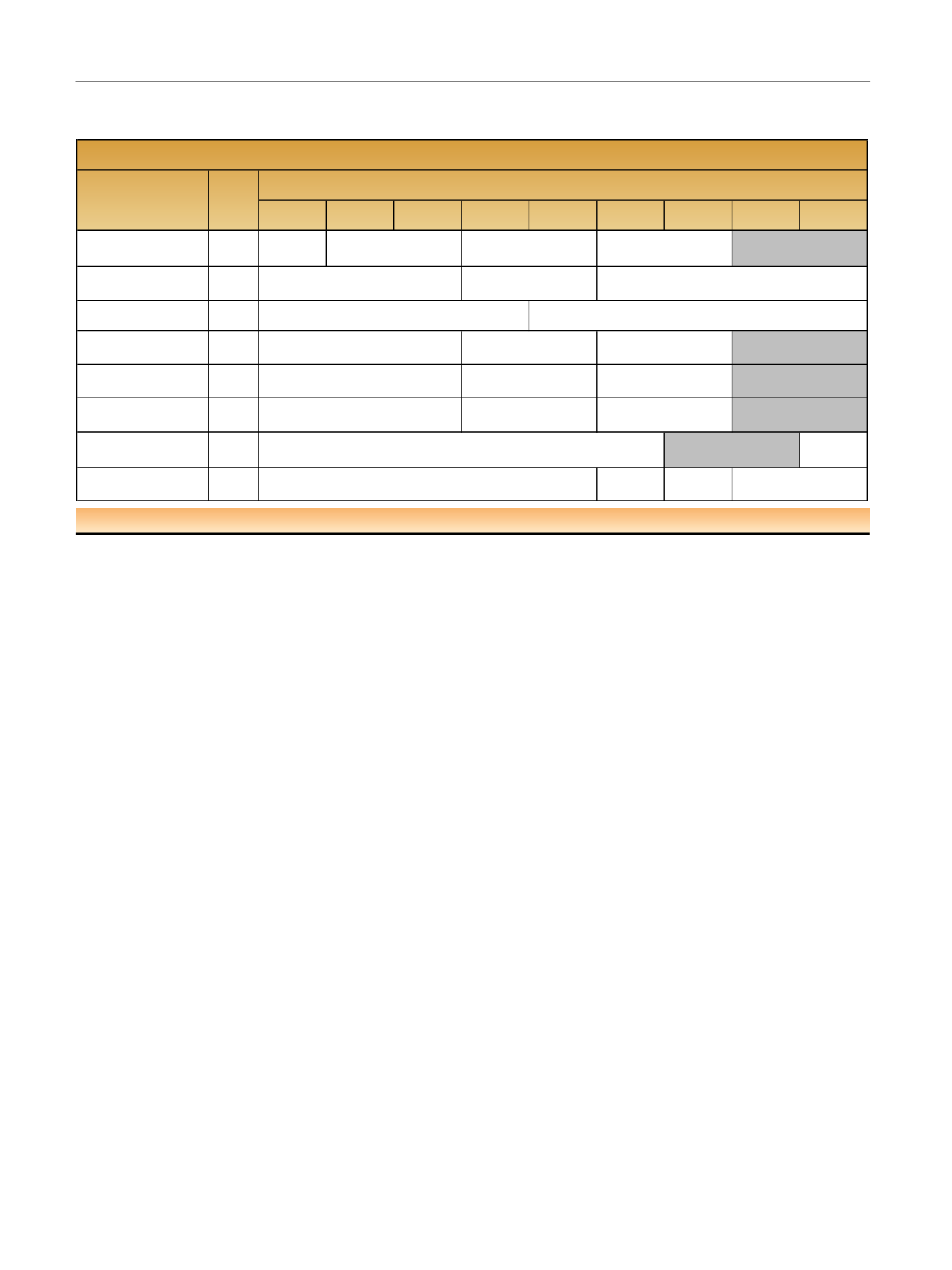
Table 4 – Multivariate analysis evaluating impact of age on cancer specific survival rates per age group and per study. The studies in grey
represent the studies where a significant difference was observed between younger and older patients
50
–
54
<50
55
–
59
60
–
64
65
–
69
70
–
74
75
–
79
80
–
84
≥85
Chromecki et al [21] 2012
ref (
N
= 321)
4429
Dalbagni et al [19] 2001
297
Dotan et al [31] 2007
1586
Fairey et al [16] 2012
2263
Patel et al [17] 2015
804
Nielsen et al [28] 2007
888
Morgan et al [23] 2012
3170
1.32 (95%
CI:0.91
-
Leveridge et al [15] 2015
ref (
N
= 582)
1701
1.02(95%
CI:0.93
-
1.26)
0.87(95%CI:0.68
-
1.13)
(
N
= 846)
ref (
N
= 1613)
1.24(95%CI:1.05
-
1.46,
p
= 0.009) (
N
= 1406)
NR
1.02 (95%CI:0.87
-
1.19,
p
= 0.522) (
N
= 578)
ref (
N
= 150)
1.24 (95%CI:0.86
-
1.80)
(
N
= 245)
1.36(95%CI:0.96
-
1.90)
(
N
= 339)
2.54(95%CI:1.62
-
3.96)
(
N
= 70)
ref (
N
= 240)
1.226 (0.884
-
1.700,
p
= 0.222) (
N
=331)
1.296(95%CI:0.921
-
1.823,
p
= 0.136) (
N
= 266)
1.742(1.015
-
2.990,
p
= 0.044) (
N
= 51)
1.56 (95%CI:1.09
-
2.24)
(
N
= 181)
ref (
N
= 557)
0.96 (95%CI:0.74
-
1.26)
(
N
= 679)
Cancer specific survival
N
Author
Trials with radical cystectomy
0.795 (95%CI:0.610
-
1.044,
p
= 0.1)(
N
= 815)
0.979 (95%CI:0.766
-
1.252,
p
= 1.252) (
N
= 1595)
1.128 (95%CI:0.880
-
1.446,
p
≤ 0.341)
1.763 (95%CI:1.238
-
2.424,
p
< 0.001) (
N
= 275)
ref (
N
= 73)
1.137 (95%CI:0.605
-
2.137,
p
= 0.6890) (
N
= 106)
1.117 (95%CI:0.619
-
2.017,
p
= 0.7135) (
N
= 118)
ref (
N
= 613)
1.26 (95%CI:0.91
-
2.017,
p
= 0.14) (
N
= 973)
CI = confidence interval; OR = odds ratio; NR = not reported; Ref = reference.
E U R O P E A N U R O L O G Y 7 3 ( 2 0 1 8 ) 4 0 – 5 0
46
















