
Except for POM, the reported incidence of morbidity
after RC is acceptable in elderly patients. However, these
results should be interpreted with caution. It is important to
point out the shortage of data on both long-term results of
cystectomy and maintenance of autonomy after surgery in
the elderly patients.
Two studies reported lower incidence of late morbidity
in older patients
[7,35]. Patients included in both trials
underwent a rigorous preoperative physical examination
and screening to ensure adequate performance status prior
to surgery.
Our findings are different from the conclusions drawn by
Froehner et al
[67]. They reported an increased risk in
perioperative morbidity in elderly patients, particularly
when an extended postoperative period (90 d instead of
30 d) is applied. Also, the continence rates after orthotopic
urinary diversion is impaired in an older population
[67]. Our paper differs from the paper of Froehner et al
[67]in several aspects, which might explain these conflict-
ing observations. First, only papers including
>
100 patients
were selected for this review in contrast to the paper of
Froehner et al
[67], where also smaller reports were taken
into consideration. Secondly, no clear age cut-off was
defined by Froehner et al
[67].
This systemic review is not free of shortcomings. The
major limitations of our systematic review are the
limitations of the literature itself. The retrospective nature
of the implemented data, the low number of articles with an
acceptable quality (Supplementary Table 1), as well as the
heterogeneity of the studies makes drawing conclusions
difficult. Differences in tumor stage at presentation and use
of perioperative chemotherapy can have an impact on
outcome as previously mentioned. Unfortunately, tumor
stage and administration of neo-adjuvant chemotherapy
were not reported in detail in the majority of the included
papers.
Taking into account that elderly patients are often denied
curative treatment and recognizing the lack of information
on performance status and presence of comorbidities we
cannot exclude that we compare the best older patients
with the average younger patients. Some evidence exists to
suggest that the accuracy of death certificates could
decrease with the age of the patient
[68]. However, it
should be remembered that the accuracy of cause of death is
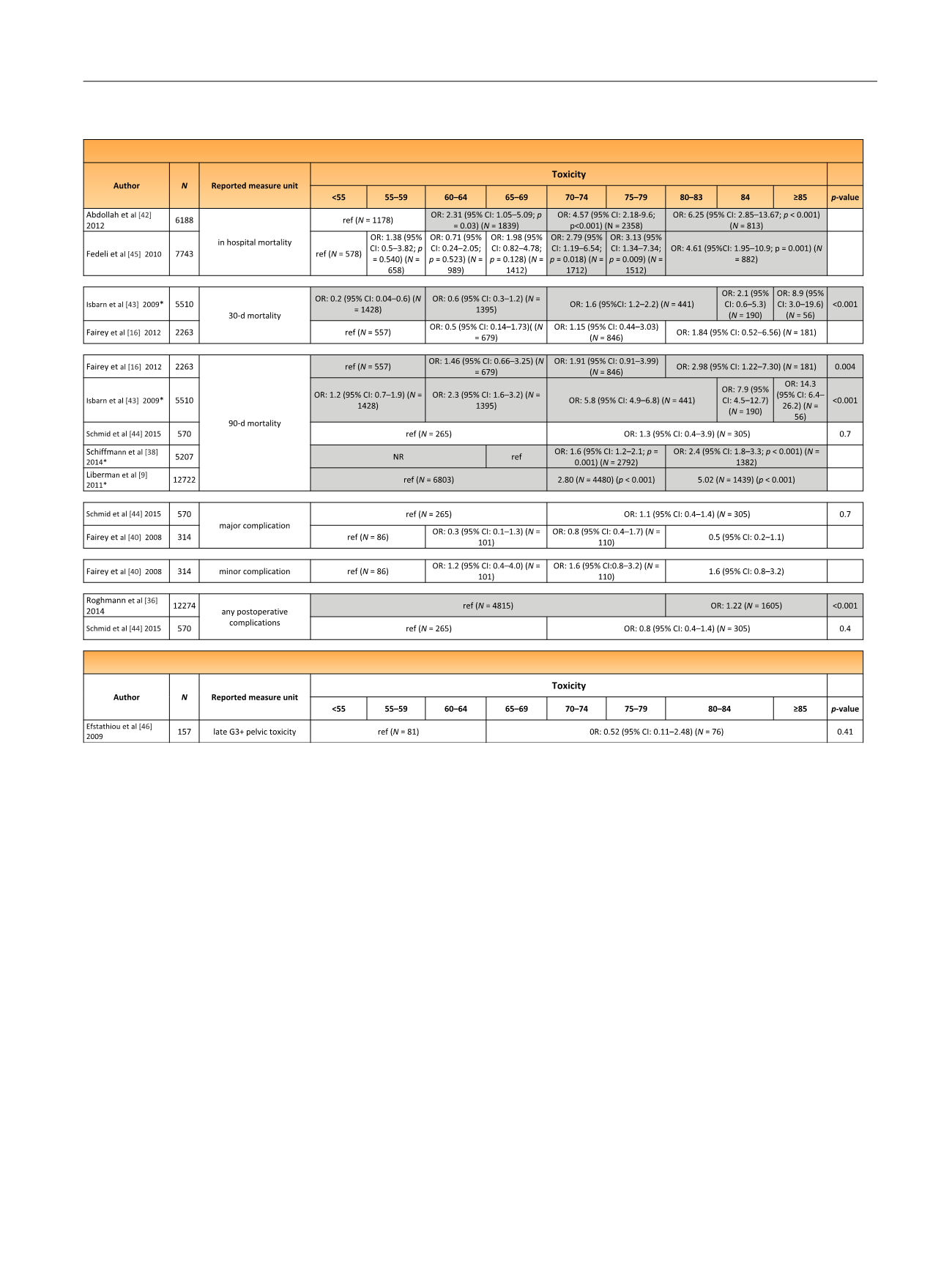
Table 5 – Multivariate analysis evaluating impact of age on morbidity rates per age group and study. The studies in grey represent the studies
where a significant difference was observed between younger and older patients
Trials with radiotherapy
Trials with radical cystectomy
E U R O P E A N U R O L O G Y 7 3 ( 2 0 1 8 ) 4 0 – 5 0
47
















