
generally higher for cancer diagnoses than other common
causes of death
[69] .Consequently, the reduction in
accuracy due to age would be expected to represent only
a small decrement in cancer cause of death accuracy.
Equally important is to recognize that for patients
deemed unsuitable for curative treatment the option of
less aggressive therapies should be regarded. External beam
radiotherapy alone can be considered as a therapeutic
option when the patient is unfit for cystectomy or
multimodality bladder-preserving approach
[70]. Short
radiotherapy regimens have been proposed for elderly
patients as an alternative for longer radiotherapy schedules
and result in acceptable toxicity with median relapse free
survival rates of 15–16 mo
[71]. A palliative cystectomy
should be considered for symptom relief if no other options
are available
[2] .5.
Conclusions
Although a proportion of elderly patients with MIBC will
benefit from curative treatment, we observed that OS, CSS,
and POM significantly worsen with age. Further prospective
studies evaluating GAs are critically needed to optimise
MIBC management in the elderly.
Author contributions:
Vale´rie Fonteyne had full access to all the data in
the study and takes responsibility for the integrity of the data and the
accuracy of the data analysis.
Study concept and design:
Fonteyne, Ost, Ploussard.
Acquisition of data:
Fonteyne, Ost.
Analysis and interpretation of data:
Fonteyne, Ost.
Drafting of the manuscript:
Fonteyne.
Critical revision of the manuscript for important intellectual content:
Ost,
Bellmunt, Droz, Mongiat-Artus, Inman, Paillaud, Saad, Ploussard.
Statistical analysis:
Fonteyne, Ost.
Obtaining funding:
None.
Administrative, technical, or material support:
None.
Supervision:
Ploussard.
Other:
None.
Financial disclosures:
Vale´rie Fonteyne certifies that all conflicts of
interest, including specific financial interests and relationships and
affiliations relevant to the subject matter or materials discussed in the
manuscript (eg, employment/affiliation, grants or funding, consultan-
cies, honoraria, stock ownership or options, expert testimony, royalties,
or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor:
None.
Appendix A. Supplementary data
Supplementary data associated with this article can be
found, in the online version, at
http://dx.doi.org/10.1016/j. eururo.2017.03.019 .References
[1]
Antoni S, Ferlay J, Soerjomataram I, Znaor A, Jemal A, Bray F. Bladder cancer incidence and mortality: a global overview and recent trends. Eur Urol 2016;71:96–108.[2]
Witjes JA, Lebret T, Compe´rat EM, et al. Updated 2016 EAU guide- lines on muscle-invasive and metastatic bladder cancer. Eur Urol 2017;71:462–75.[3]
Extermann M, Aapro M, Bernabei R, et al. Use of comprehensive geriatric assessment in older cancer patients: recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit Rev Oncol Hematol 2005;55:241–52.[4] Moga C, Schopflocher D, Hartstall C. Development of a quality
appraisal tool for case series studies using a modified Delphi
technqiue. Institute of Health Economics.
http://www.ihe.ca .[(Fig._2)TD$FIG]
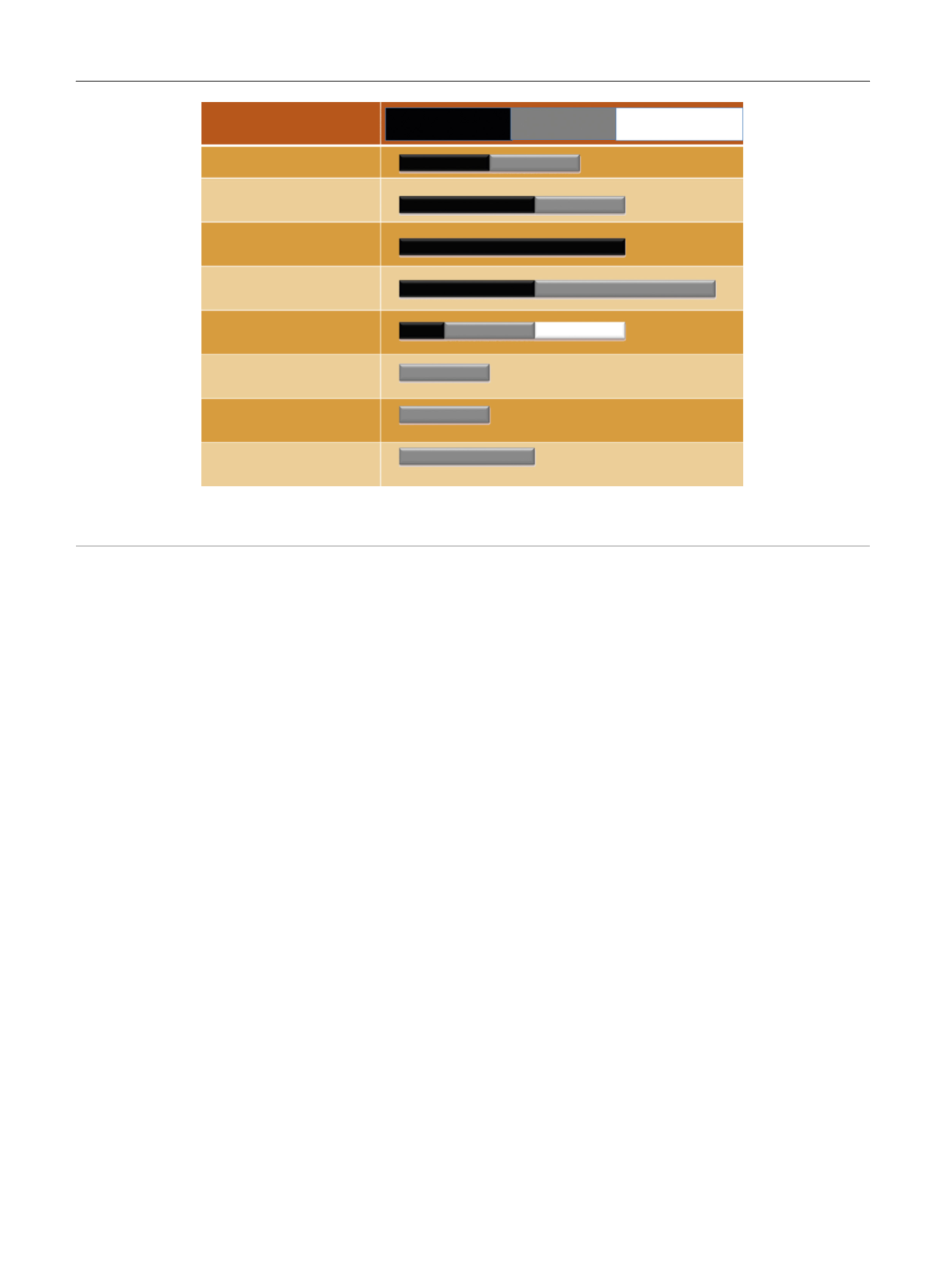
Safety outcome
Peri-operative mortality
30-d mortality
90-d mortality
Early complications
Late complications
Minor complications
Major complications
Overall complication rate
1 (36)
3 (35, 36, 39)
(15, 16, 30, 38, 41)
3 (15, 34, 38)
2 (27, 36) a
3 (11, 18, 34)
2 (8, 30)
2 (8, 30)
2 (12, 27)
4 (7, 12, 27, 37)
2 (7, 16)
2 (7,35)
2 (7, 35)
a
a
5
Old worse than
young
Young worse than
old
Old = young
Fig. 2 – Incidence of morbidity in old (>70 yr) versus young patients (<70 yr). The numbers represent the number of articles.
a
Two trials compared octogenarians with younger patients (<80 yr).
E U R O P E A N U R O L O G Y 7 3 ( 2 0 1 8 ) 4 0 – 5 0
48
















